WASHINGTON, DC — Lung cancer remains the leading cause of cancer death in the U.S. and among veterans, who face an increased risk of developing the malignancy. Consequently, the VA actively screens for the disease and continues to expand access to new treatment options.
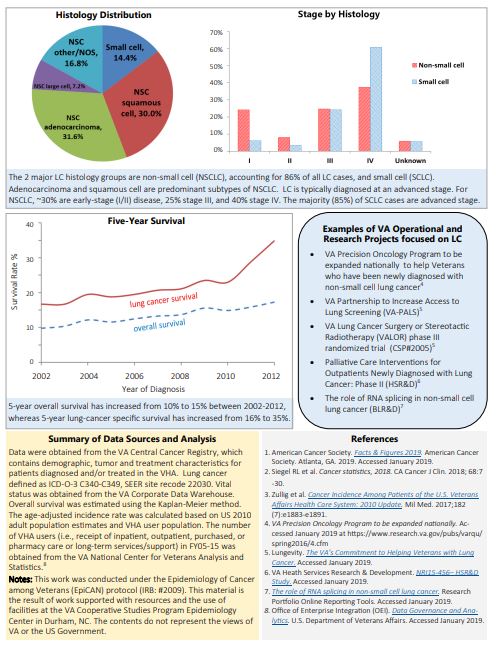
Lung cancer has two primary types: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). While the names distinguish the two types based on the distinctive appearance of the cancer cells under a microscope, the differences between SCLC and NSCLC extend into their incidence, location, aggressiveness and treatments as well.
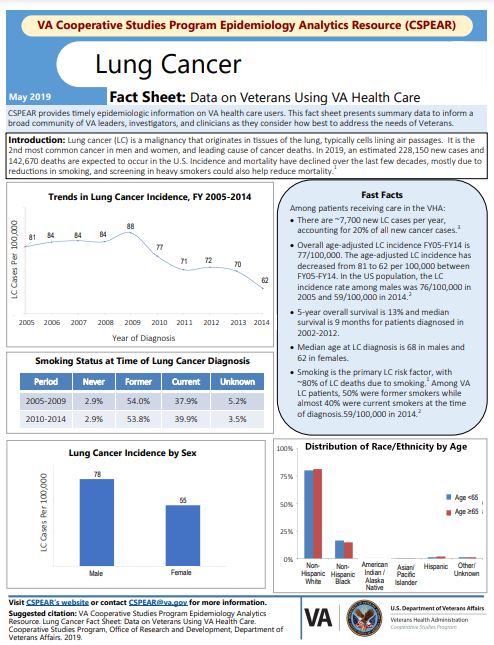
Nationally, NSCLC represents 85% of all lung cancers: SCLC accounts for 10% to 15%, with a small number of cancers exhibiting characteristics of both NSCLC and SCLC.
The same split is seen in the veteran population. Of the nearly 8,000 veterans who are diagnosed with lung cancer each year, about 7,000 have NSCLC and 1,000 have SCLC, according to the VA Cooperative Studies Program Epidemiology Analytics Resource.
Like NSCLC, SCLC is a presumptive condition for veterans exposed to Agent Orange or other herbicides during the Vietnam era and in the Korean demilitarized zone, as well as those exposed to radiation. SCLC is also presumed to be service-related in veterans who served in Southwest Asia and other combat zones where they were exposed to fine particulate matter and burn pits.
Veterans are also at particular risk for SCLC due to older average age and higher rates of smoking than the general population. Among veterans with all types of lung cancer, 53.8% were former smokers and 39.9% were current smokers at the time of diagnosis. Exposure to carcinogens like asbestos and PFAS chemicals as well as air pollution also increases risk.1
The U.S. Preventive Services Task Force and VA guidelines recommend screening for all lung cancers with low-dose CT scans in adults aged 50 to 80 years who have a 20 pack-per-year history of smoking and either still smoke or quit within the last 15 years. Implementation of the screening guidelines has increased the diagnosis of lung cancer in the VA and enabled more veterans with early stage NSCLC to receive curative treatment.
The SCLC Challenge
Click to Enlarge
The situation is less rosy with SCLC, however. SCLC stands out for its rapid spread and often late diagnosis. While SCLC can be treated, it often recurs as it has frequently metastasized before it is detected. A new therapy, tarlatamab-dlle, recently gained U.S. FDA approval and offers a powerful option for patients facing recurrence.
SCLC typically starts in the bronchi and then often spreads quickly to the lymph nodes and beyond. Common locations for metastases include the adrenal glands, bones, brain and liver.
As part of staging the disease, SCLC is categorized as being either limited stage or extensive stage at diagnosis. In limited-stage disease, the cancer remains in one lung, though it may have invaded lymph nodes on the same side or the nearby supraclavicular or mediastinal lymph nodes. Most importantly, the cancer is confined to a small enough region that it can be treated with radiation treatment in just one area.
In extensive-stage disease, the cancer spreads throughout the lung, to both sides or metastasizes to other parts of the body. Extensive-stage SCLC may also involve the fluid surrounding the heart and lungs.
Common symptoms of SCLC include a persistent cough, difficulty breathing, chest pain, hoarseness and weight loss. Some patients may also cough up blood or experience swelling in the face and neck or neurological issues due to metastasis. Diagnosing SCLC involves imaging such as chest X-rays or CT scans, followed by a biopsy to confirm the presence of cancer cells. Additional tests, like PET scans, help stage the cancer and determine how far it has spread.
Despite advances, long-term survival for SCLC remains poor, with most patients surviving two to four months without treatment.
Patients with limited-stage disease who undergo chemotherapy and thoracic radiation therapy (TRT) experience significantly longer survival, a median survival of 16 to 24 months, but the five-year survival rate remains low at 14%. For those with extensive-stage SCLC, median survival drops to six to 12 months, and long-term survival is rare.
Among veterans diagnosed with SCLC, nearly 15% are diagnosed with limited disease (stage I or II); 85% already have extensive-stage, advanced disease when first detected.
Treatment for SCLC at VA
The VA offers veterans a wide range of treatments for SCLC, from chemotherapy and radiation therapy to cutting-edge immunotherapy and combinations of these modalities. Because most cases have already spread, surgery is not recommended in SCLC. Many patients with SCLC initially respond well to therapy, but the malignancy tends to return and become treatment resistant.
A new therapy, tarlatamab-dlle, that addresses this gap gained FDA accelerated approval in May. Tarlatamab-dlle is indicated for treatment of extensive-stage small cell lung cancer in patients who experienced disease progression after platinum-based chemotherapy. A bispecific T-cell engager (BiTE) immunotherapy, tarlatamab-dlle received approval based on its overall response rate and duration of response in clinical trials. Prior to approval, the FDA granted tarlatamab-dlle priority review, breakthrough drug designation, and orphan drug designation, demonstrating its significance for patients with limited options.
The VA’s Precision Oncology Program and partnerships with leading cancer research institutions help ensure that veterans receive state-of-the-art care for SCLC. These collaborations have increased access to genetic testing, allowing doctors to tailor treatments to individual patients. New treatments, like tarlatamab-dlle, reflect the VA’s commitment to bringing cutting-edge therapies to veterans with advanced SCLC.
While the outlook for SCLC remains challenging, especially for veterans with extensive-stage disease, the VA’s focus on improving diagnostic tools, early detection and integrating new therapies offers hope for better outcomes.
- VA Cooperative Studies Program Epidemiology Analytics Resource. Lung Cancer Fact Sheet: Data on Veterans Using VA Health Care.