
In Afghanistan in 2014, U.S. Air Force Senior Airman Freddy Toruno, 455th Expeditionary Medical Support Squadron diagnostic imaging technologist, positioned a servicemember for a CT scan to diagnosis traumatic brain injury at Bagram Air Field’s Craig Joint Theater Hospital. U.S. Air Force photo by Staff Sgt. Evelyn Chavez.
BETHESDA, MD — Traumatic brain injury, especially involving penetration, significantly increased the risk for atrial fibrillation or atrial flutter in U.S. military servicemembers and veterans, according to a new study.
The Uniformed Services University of Health Sciences-led authors called for further work to “delineate the long-term risk of arrhythmias after TBI.” Researchers from the VA Salt Lake City Healthcare System were also on the study team.
The report in Heart Rhythm explained, “Traumatic brain injury (TBI) is associated with a variety of adverse long-term outcomes and increases sympathetic nervous system activation which could increase the risk of arrhythmias including atrial fibrillation or atrial flutter (AF/AFL).”1
The researchers sought to examine episodes of TBI and subsequent AF/AFL in a large cohort of post-9/11 servicemembers and veterans.
The focus was on TBI, stratified by severity (mild, moderate/severe and penetrating), with the outcome defined as a subsequent diagnosis of AF/AFL. Participants included more than 1.9 million veterans, 19.2% of whom experienced an episode of documented TBI. Most were young (63% less than 35 years), male (81.7%) and non-Hispanic white (62.7%).
Their results indicated that AF/AFL was diagnosed in 22,087 subjects. The researchers explained that, on univariate analysis, only penetrating TBI (hazard ratio [HR] 2.02, 95% confidence interval [CI] 1.84-2.23; p<0.001) was associated with AF/AFL compared to veterans without TBI.
“After adjustment in the full multivariable model (adjusted for age, sex, race and ethnicity, service branch, rank, component and comorbidities), mild (HR 1.27, 95% CI 1.22-1.32; p<0.001), moderate/severe (HR 1.34, 95% CI 1.24-1.44; p<0.001), and penetrating TBI (HR 1.82, 95% CI 1.65-2.02; p<0.001) were significantly associated with AF/AFL compared to no TBI,” they added. “Post-hoc analyses demonstrated that the risk of AF/AFL was concentrated in female and younger patients.”
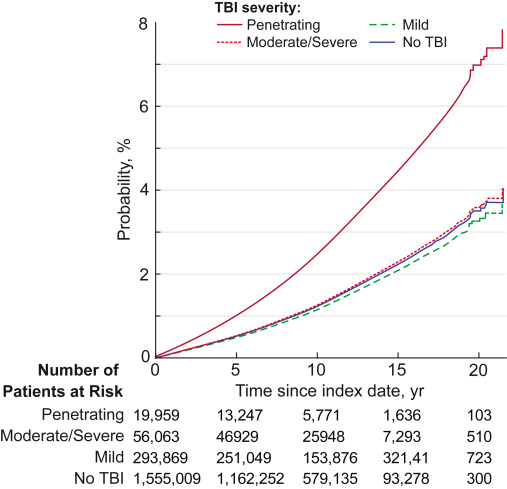
Click to Enlarge: Cumulative incidence functions for atrial fibrillation/flutter stratified by traumatic brain injury (TBI) severity. The development of the outcome (atrial fibrillation and flutter) is demonstrated by TBI group: no TBI (continuous blue), mild TBI (dashed green), moderate/severe TBI (dashed red), and penetrating TBI (continuous dark red). Source: Heart Rhythm Society
TBI is a common injury sustained in the course of military service. Since 2000, 492,167 servicemembers have had a TBI, according to the study. “Emerging evidence indicates that far from being an acute event, TBI is a chronic disease that is associated with a variety of adverse long-term outcomes,” the authors wrote. “Among these adverse outcomes are recognized risk factors for atrial fibrillation or atrial flutter (AF/AFL), including hypertension, diabetes, hyperlipidemia, cardiovascular disease, obesity and obstructive sleep apnea.”
They added that, in addition to classic risk factors for AF/AFL, TBI has been associated with the subsequent development of post-traumatic stress disorder (PTSD), which is itself a risk factor for AF/AFL. The risk for the condition also is increased in patients with spinal cord injury and traumatic intracranial hemorrhage, as well as other injuries in combat casualties, according to the report.
“Given the association between TBI and known risk factors, as well as the association between AF/AFL and other traumatic injuries, we hypothesized that servicemembers and veterans with a history of TBI would be more likely to develop AF/AFL compared to their uninjured counterparts,” the study team advised, saying the hypothesis was tested using data from the Long-Term Impact of Military Relevant Brain Injury Consortium-Chronic Effects of Neurotrauma Consortium (LIMBICCENC), a large retrospective study of post-9/11 servicemembers and veterans.
Traditionally Low-Risk Groups
“While all levels of TBI were associated with AF/AFL in the adjusted models, only penetrating TBI was associated with AF/AFL in the bivariate model,” the researchers pointed out. “On post-hoc analysis, we found that this was due to differences in risk between subgroups (female vs. male and young vs. older). These results imply that the risk imparted by TBI on subsequent AF/AFL is concentrated in traditionally low-risk groups (female and younger subjects).”
They advised that the pathogenesis of AF/AFL following TBI remains unclear but wrote that one hypothesis “is that damage to the structures of the brain that are central in the regulation of the autonomic nervous system leads to excessive catecholamine release and subsequent arrhythmias. An increase in pressure due to damage triggers stimulation of the sympathetic autonomic nervous system through the insular cortex and hypothalamus, leading to activation of the adrenal glands, release of catecholamines, and increased sympathetic stimulation of the heart.”
Adding that this is thought to be a neuroprotective mechanism for maintaining blood flow to the brain following injury, the authors added, “This catecholamine storm can perpetuate neurogenic stunned myocardial syndrome, the result of which causes damage to myocytes through depletion of adenosine triphosphate (ATP), thus leading to cell death, heart failure, and the triggering of AF.”
They suggested another mechanism for the arrhythmia-inducing effects of catecholamines could be that the increase in sympathetic stimulation of the heart results in an increase in cytosolic calcium levels in myocardial cells, with other theories involving the parasympathetic autonomic nervous system, vagal nerve stimulation and the body’s inflammatory response following TBI.
“Prior work from our group in this cohort of patients demonstrated that subjects with TBI were at a higher risk for cardiovascular disease, a well-known risk factor for AF/AFL,” according to the researchers. “Other work has shown that TBI increases the risk for other traditional AF/AFL risk factors, including hypertension, diabetes, hyperlipidemia and obesity. Furthermore, TBI has also been shown to increase rates of obstructive sleep apnea4 and PTSD, both of which are emerging as risk factors for AF/AFL. While our analysis controlled for these variables at baseline, further work is needed to evaluate if other risk factors are in the pathway between TBI and AF/AFL.”
An unexpected result was that the impact of TBI was most pronounced in female and younger subjects, groups with lower overall risk of AF/AFL. “The exact reason for these effects is unclear, but these results closely mirror findings from other recent work that conducted gender stratification of mild TBI effects among deployed veterans, which identified both intrinsic and extrinsic gender differences in risk for adverse outcomes after TBI,” they advised.
They added, “Understanding how risks in females may differ from their male counterparts is important for the long-term care of injured servicemembers.”
- Stewart IJ, Howard JT, Amuan ME, Kennedy E, et. Al. Traumatic Brain Injury is Associated with the Subsequent Risk of Atrial Fibrillation or Atrial Flutter. Heart Rhythm. 2024 Sep 13:S1547-5271(24)03316-2. doi: 10.1016/j.hrthm.2024.09.019. Epub ahead of print. PMID: 39278610.
