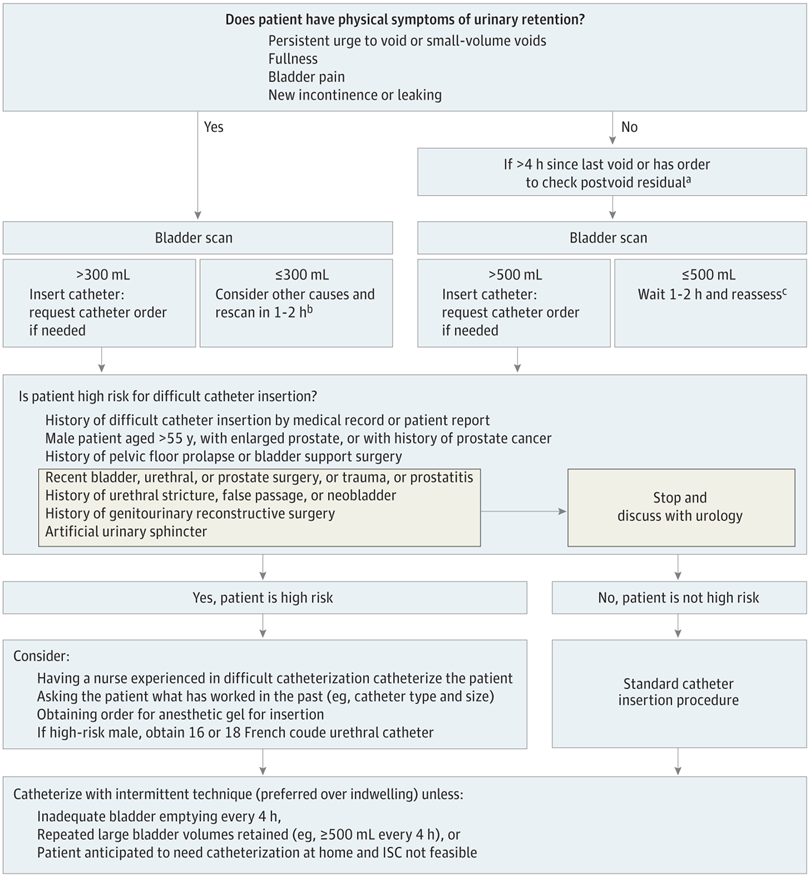
Click to Enlarge: The algorithm is intended for the inpatient setting. Cutoffs were determined based on a combination of literature review, expert opinion, and local practice patterns. Of note, use of external catheters to treat urinary retention is inappropriate as external catheters only collect spontaneously voided urine. ISC indicates intermittent straight catheter.
a. Consider checking sooner if the patient is receiving high volumes of intravenous fluid or diuretics.
b. Other common causes of these urinary symptoms include urinary tract infection, overactive bladder, small bladder capacity, or recent catheterization. Consider contacting attending physician for further evaluation.
c. Evaluate the patient’s fluid intake and consider increasing fluids. Call attending physician if urine output is less than 35 mL per hour, raising concern for oliguria from hypovolemia or acute kidney injury. Source JAMA Network Open
ANN ARBOR, MI — A new algorithm could improve care for adult inpatients who need to be evaluated for urinary retention and possible catheterization, according to a recent study.
The study published in JAMA Network Open aimed to develop an algorithm for screening and management of urinary retention among adult inpatients. The study authors are affiliated with the VA Ann Arbor (MI) Healthcare System and the University of Michigan.1
Acute urinary retention “is common, but variations in diagnosis and management can lead to inappropriate catheterization and harm,” the authors explained. “While urinary catheters are frequently used in hospitalized medical and surgical patients, there are no guidelines or widely accepted algorithms for screening and management of urinary retention in these patients.”
The researchers suggested the necessity of balancing the potential complications of untreated urinary retention (e.g., pain, bladder dysfunction) against those of urinary catheterization (e.g., urethral injury, urinary tract infection) when deciding whether to insert a catheter. They pointed out that, although urinary retention algorithms exist for outpatient populations, there’s limited evidence to guide management in hospitalized patients.
In this mixed-methods study, an 11-member multidisciplinary expert panel of nurses and physicians from across the United States used the RAND/UCLA Appropriateness Method and qualitative interviews to develop a urinary retention algorithm. From March 2015 to May 2015, they rated 107 clinical scenarios involving diagnosis and management of adult urinary retention in postoperative and medical inpatients. The panel ratings informed the first algorithm draft. Then, semi-structured interviews were conducted from October 2020 to May 2021 with 33 frontline clinicians, nurses and surgeons from five Michigan hospitals to gather feedback and inform algorithm refinements.
“Managing urinary retention can be difficult because healthcare providers are trying to balance the potential complications of not treating their patient’s urinary retention, such as pain and bladder dysfunction, with the potential complications of treating retention with a urinary catheter, such as urethral injury or urinary tract infection,” Jessica Ameling, MPH, a co-author of the study and research area specialist in the University of Michigan’s Division of General Medicine, told U.S. Medicine. “Our study produced a guideline that balances these two risks and can help healthcare professionals provide safe, standardized care. For example, we found that intermittent catheterization was preferred to indwelling (“Foley”) catheterization for managing lower bladder volumes.”
Ameling said the study is unique “in that we used two methods to develop this urinary retention evaluation and catheterization algorithm. In the first phase, we convened experts in the field to review the published literature on this topic and provide evidence-based expert recommendations. Then, we used these results to develop an algorithm that we showed to clinicians in the field to make sure the algorithm was practical and understandable.”
The final algorithm, she said, “provides guidance to clinicians on what urinary retention symptoms to look out for in their patients, how long to wait before bladder scanning their patients, when it is appropriate to wait and reassess vs. catheterize their patient, and guidance on safe catheter placement if a catheter is needed.”
The study had several major findings. First, the authors found that “bladder scanners were preferred over catheterization for urinary retention diagnosis in symptomatic patients or starting as soon as three hours since last void if asymptomatic. Second, bladder scanner volumes appropriate to prompt catheterization were 300 mL or greater in symptomatic patients and 500 mL or greater in asymptomatic patients. Lastly, intermittent was preferred to indwelling catheterization for managing lower bladder volumes,” Ameling pointed out.
Study authors recommended that hospitals incorporate the algorithm into their quality improvement initiatives and made it visually appealing to allow busy clinicians to navigate through it easily.
“Some implementation ideas that worked at other hospitals include placing laminated copies of the algorithm at the nurses’ stations and/or connecting them to the unit bladder scanners so that clinicians can easily access it when they are making these decisions for their patient,” Ameling explained. “We also recommend the ubiquitous presence of bladder scanners in hospitals to allow for rapid, noninvasive diagnosis and prevent unnecessary catheterization. For patients, it’s important to remember that acute (sudden) urinary retention is serious, and they should follow their healthcare provider’s care plan.”
The authors sought to improve acute urinary retention evaluation and develop an algorithm because they saw a clinical need.
“In our previous work, we found that the management of urinary retention was really the “Wild West”—it was all over the place,” Ameling said. “And this unstandardized care could lead to patient harm, such as untreated urinary retention or the use of indwelling urinary catheters—an invasive medical device which can cause patient harm—when they may not be needed.”
“Physicians and nurses told us that they wanted a standardized way to manage urinary retention so that everyone was on the same page,” she added. “They also wanted discrete “cutoffs” to let them know, for example, when a patient is retaining a certain amount of urine, that it is appropriate to use a urinary catheter.”
- Chrouser K, Fowler KE, Mann JD, Quinn M, Ameling J, Hendren S, Krapohl G, Skolarus TA, Bernstein SJ, Meddings J. Urinary Retention Evaluation and Catheterization Algorithm for Adult Inpatients. JAMA Netw Open. 2024 Jul 1;7(7):e2422281. doi: 10.1001/jamanetworkopen.2024.22281. PMID: 39012634; PMCID: PMC11252892.

