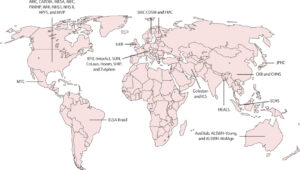
Click to Enlarge: ALSWH=Australian Longitudinal Study on Women’s Health. ARIC=Atherosclerosis Young Adults Study. AusDiab=Australian Diabetes, Obesity and Lifestyle Study. CARDIA=Coronary Artery Risk Development in Young Adults. CHNS=China Health and Nutrition Survey. CKB=China Kadoorie Biobank. CoLaus=Cohorte Lausannoise Study. COSM=Cohort of 50 000 Swedish Men. ELSA-Brasil=Brasilian Longitudinal Study of Adult Health. EPIC=European Prospective Investigation into Cancer. FMC=Finnish Mobile Clinic Health Examination Survey. HEALS=Health Effects of Arsenic Longitudinal Study. Golestan=The Golestan Cohort Study. Hoorn=Hoorn Study. HPFS=Health Professionals Follow-up Study. ICS=Isfahan Cohort Study. JPHC=Japan Public Health Center-based Prospective Study. MEC=Multiethnic Cohort Study. MESA=Multi-Ethnic Study of Atherosclerosis. MTC=The Mexican Teachers’ Cohort. MVP=Million Veteran Program. NHS=Nurses’ Health Study. PRHHP=Puerto Rico Heart Health Program. SCHS=Singapore Chinese Health Study. SHIP=Study of Health in Pomerania. SMC=Swedish Mammography Cohort. SUN=Seguimiento Universidad de Navarra cohort study. UKB=UK Biobank. WHI=Women’s Health Initiative Study. Zutphen=Zutphen Elderly Study.
Source: The Lancet
CAMBRIDGE, UK — Consuming meat, especially processed and red meat, is a risk factor for the development of type 2 diabetes, according to a new study involving VA researchers.
“These findings highlight the importance of reducing meat consumption for public health and should inform dietary guidelines,” according to the study led by the University of Cambridge School of Clinical Medicine in the UK and co-authors, including researchers from the Veterans Epidemiology Research and Information Center (MAVERIC) at the VA Boston Healthcare System,
The study published in The Lancet Diabetes & Endocrinology raised the question of whether meat consumption could increase the risk of type 2 diabetes. “However, evidence is largely based on studies of European and North American populations, with heterogeneous analysis strategies and a greater focus on red meat than on poultry,” the authors wrote. “We aimed to investigate the associations of unprocessed red meat, processed meat, and poultry consumption with type 2 diabetes using data from worldwide cohorts and harmonized analytical approaches.”
The individual-participant federated meta-analysis involved data from 31 cohorts participating in the InterConnect project. Cohorts were from the region of the Americas (n=12) and the Eastern Mediterranean (n=2), European (n=9), South-East Asia (n=1), and Western Pacific (n=7) regions.
Each cohort provided access to individual-participant data; participants were eligible for inclusion if they were aged 18 years or older and had available data on dietary consumption and incident type 2 diabetes and were excluded if they had a diagnosis of any type of diabetes at baseline or missing data.
Among more than 1.96 million adults eligible for participation, 107, 271 incident cases of type 2 diabetes were identified during a median follow-up of 10 (IQR 7-15) years. The study found that median meat consumption across cohorts was 0-110 g/day for unprocessed red meat, 0-49 g/day for processed meat, and 0-72 g/day for poultry.
“Greater consumption of each of the three types of meat was associated with increased incidence of type 2 diabetes, with HRs of 1·10 (95% CI 1·06-1·15) per 100 g/day of unprocessed red meat (I2=61%), 1·15 (1·11-1·20) per 50 g/day of processed meat (I2=59%), and 1·08 (1·02-1·14) per 100 g/day of poultry (I2=68%),” the researchers reported. “Positive associations between meat consumption and type 2 diabetes were observed in North America and in the European and Western Pacific regions; the CIs were wide in other regions.”
The authors pointed out that no evidence was found that the heterogeneity was explained by age, sex, or BMI. “The findings for poultry consumption were weaker under alternative modeling assumptions,” they added. “Replacing processed meat with unprocessed red meat or poultry was associated with a lower incidence of type 2 diabetes.”
Surpasses Optimal Dietary Guidelines
Background information in the article advised that global meat production has increased quickly over the last half-century. One result is that dietary meat consumption surpasses optimal guidelines in many regions and “is correlated with an elevated burden of non-communicable diseases, including type 2 diabetes,” the researchers wrote.
Type 2 diabetes affects more than 500 million people worldwide and is estimated to affect 1 billion people by 2050, the study noted, adding that evidence from several meta-analyses of published prospective studies have demonstrated a positive association between unprocessed red meat and processed meat consumption and the heightened risk of type 2 diabetes.
On the other hand, some reviews have drawn contradictory conclusions on the certainty of evidence in this field.
“Specifically, some studies concluded that the current evidence is weak and of low certainty for guiding dietary recommendations to limit meat consumption,” the authors recounted. “These conclusions were derived from similar published data and results to other meta-analyses, but the data were interpreted differently (eg. without considering biological mechanisms) and through different evidence-grading approaches (such as the burden of proof approach or the GRADE approach, which are potentially influenced by epidemiological biases and potential conflicts of interest cannot be ruled out.”
The study also described how poultry has often been considered a potentially healthier alternative to red and processed meat. In fact, the association between poultry consumption and type 2 diabetes risk has been described in only a few studies, with inconclusive results, according to the researchers.
They added, “Moreover, published associations between meat consumption and the incidence of type 2 diabetes have been heterogeneous, probably because of variations in research methods (such as the extent of adjustment for potential confounders and baseline-only vs repeated dietary assessment) and variations in population-specific characteristics (such as cooking methods).”
The existing evidence also shows a geographical imbalance, according to the study team, with the majority of studies from populations in the U.S. and Europe, with few from Asia and other areas, “underscoring the need for evaluation in diverse populations.”
The authors suggested that an analysis of geographically diverse data is crucial for characterizing the association between meat consumption and incident type 2 diabetes and understanding the potential sources of the heterogeneity.
“To our knowledge, no study to date has conducted a meta-analysis of individual-participant data to investigate the association between meat consumption and incident type 2 diabetes,” they wrote. “In this study, we hypothesized that intakes of unprocessed red meat and processed meat are associated with higher incidence of type 2 diabetes and that poultry consumption is not associated with risk of type 2 diabetes, and could therefore be a healthier alternative to unprocessed red meat and processed meat.”
The researchers concluded that their current findings support the notion that lowering the consumption of unprocessed red meat and processed meat could benefit public health by reducing the incidence of type 2 diabetes. Uncertainty remains regarding the positive association between poultry consumption and the incidence of type 2 diabetes, however, and they call for more investigation of that.
- Li C, Bishop TRP, Imamura F, Sharp SJ, et. Al. EPIC-InterAct Consortium; Forouhi NG, Wareham NJ. Meat consumption and incident type 2 diabetes: an individual-participant federated meta-analysis of 1·97 million adults with 100 000 incident cases from 31 cohorts in 20 countries. Lancet Diabetes Endocrinol. 2024 Sep;12(9):619-630. doi: 10.1016/S2213-8587(24)00179-7. PMID: 39174161.

