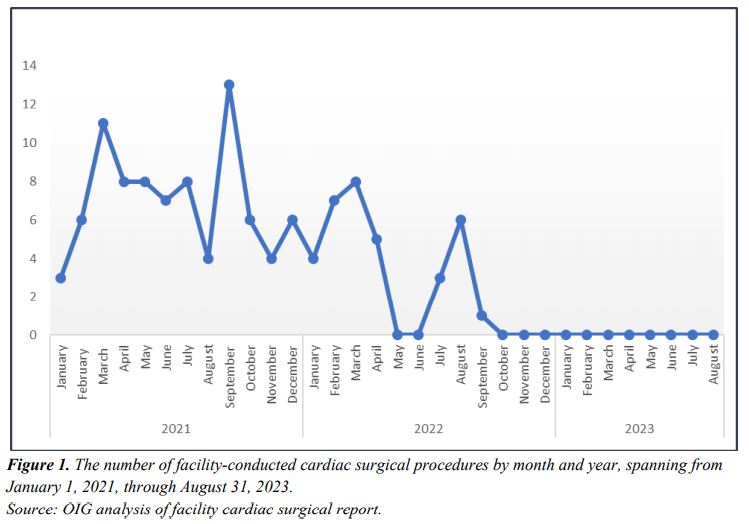
Click to Enlarge: The number of facility-conducted cardiac surgical procedures by month and year, spanning from
January 1, 2021, through August 31, 2023. Source: OIG analysis of facility cardiac surgical report.
AURORA, CO — At the Rocky Mountain Regional VAMC, a toxic work environment caused by a handful of facility leaders resulted in mass resignations by top clinical staff and the closure of its cardiothoracic surgery program, according to a report from the VA Office of the Inspector General (OIG).
The incident has legislators and VA watchdogs baffled as to how such an environment could have been allowed to fester for so long without coming to the attention of VISN or national VA leadership.
“Key senior leaders created an environment where a significant number of clinical and administrative leaders and frontline staff from a multitude of service lines felt psychologically unsafe, deeply disrespected, and dismissed, and feared that speaking up or offering a difference of opinion would result in reprisal,” the OIG investigators stated in the report.
The leaders mentioned in the report included VA Eastern Colorado Healthcare Director Michael Kilmer and his chief of staff, Shilpa Rungta, MD, as well as the deputy chief of staff for inpatient operations (DCOS-IO) and associate chief of staff for education (ACOS-E). According to testimony from employees, the director and chief of staff created a culture of fear and reprisal that valued placing blame over finding solutions. Even in town hall meetings, their demeanor was described as demeaning and condescending, according to the OIG.
Rungta also served as the interim chief of medicine service due to the long-standing vacancy in that position. The result, according to staff, was a conflict of interest and a lack of a key voice in leadership that was advocating for the needs of patients and providers, according to the OIG investigators.
In January 2023, Rungta added the DCOS-IO and ACOS-E to the hospital’s peer review committee as voting members. According to what other members of the committee told the OIG, the pair began to dominate discussions and focused on finding fault and assigning blame rather than identifying process improvements.
“Several PRC members reported that physician groups, such as hospitalists and surgeons, were targeted by key senior leaders in peer reviews,” the report stated. “Another PRC member shared that the fear of being peer-reviewed led to a hesitancy to perform high risk procedures, while another described patient safety reporting as an avenue to assign blame.”
From 2022 through 2023, there was a mass exodus by clinical staff, including the chiefs of hematology and oncology, care management and social work, cardiothoracic surgery, physical medicine and rehabilitation, anesthesiology and behavioral health, as well as several deputy chiefs and other service leaders.
The lack of staff contributed to the hospital’s inability to conduct cardiac surgeries, and the facility put all cardiothoracic surgeries on a monthlong pause in June 2022. According to the OIG, five adult critical care nurse practitioners resigned, transferred or retired in April 2022, limiting the hospitals’ ability to provide 24/7 ICU coverage. Surgeries resumed in July, but only because of staff volunteering to provide that coverage.
That fix was temporary, though, and a second pause was implemented in September 2022—one that lasted through October 2023. The facility leaders failed to notify VISN leadership or VA Central Office of this second, extended, pause. When interviewed by the OIG in July 2023, the VISN director reported a lack of awareness of any problems with the facility’s CT surgical program.
The hospital leaders also failed to notify the VISN when they resumed CT surgeries following the 11-month pause. This went against VA regulations which state that “all proposals requiring restricting, reduction, or augmentation of major clinical programs or services … must be approved by the Under Secretary for Health.”
Made aware by the OIG of the problems at the Aurora, CO, facility, in late October 2023 the VISN director detailed the facility director and chief of staff away from their facility duties “to ensure a fair and transparent investigation into the multiple concerns.”
How VISN leadership remained unaware of not only the surgical stoppage but also the larger cultural issues reportedly pervading the hospital was something that deeply troubled OIG investigators.
“[Our investigation] describes an absolute absence of VISN awareness and leadership in holding medical facility directors accountable,” said Julie Kroviak, MD, principal deputy assistant IG for Healthcare Inspections at a House VA Committee hearing. “There’s so much negative energy at that facility. … When you have that type of exodus of clinical staff; when you have closure of a cardiothoracic surgery program; when you’ve shattered a relationship with a residency program—how that noise doesn’t make it to a higher level for immediate intervention, rescue, whatever you want to call it, [we don’t know]. Our team was appropriately baffled by that story.”

