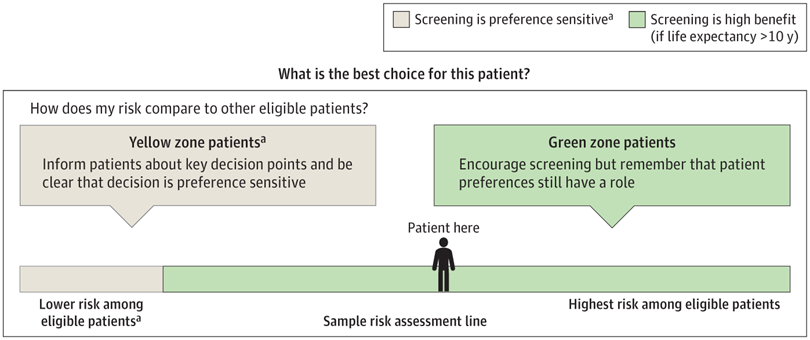
Click to Enlarge: How Clinicians Were Trained to Frame Results for High-Benefit Persons. a. Best option depends on patient preferences.
Source: JAMA Network Open
ANN ARBOR, MI — Research, including a new study of 57,000 U.S. veterans diagnosed with lung cancer, has shown that low-dose computed tomography lung cancer screening (LCS) saves lives. Yet, despite national guidelines recommending (LCS) for those meeting age and smoking criteria, less than 20% of eligible people get screened.
Moreover, recent studies indicate that uptake is poorly distributed: Veterans with high lung cancer risk and thus higher predicted benefit from LCS, including Black veterans, are less likely to be screened, and veterans with lower benefit due to poor health and limited life expectancy are more likely to be screened. Thus, it is important to identify tools that may be able to increase LCS update, especially for those with the most to gain, state authors of a new multicenter study demonstrating the effectiveness of one such approach—a shared decision-making (SDM) tool which uses prediction models to augment simple risk factor criteria.
While prediction models that effectively identify people with high lung cancer risk and high life expectancy may be an important tool for optimizing the delivery of LCS to those who have the most to gain from it, there are concerns that implementing prediction into busy primary care settings might not be feasible and could even hinder broad implementation of LCS if they were to completely replace the more traditionally used simple selection risk factor-based eligibility criteria (age 50-80, ≥20 pack-year tobacco history and <15-year quit history). For that reason, the 2021 American College of Chest Physicians (CHEST) guideline has recommended using prediction to augment rather than replace simple criteria as a way to optimize shared decision-making for high-benefit LCS candidates while still allowing for selection of a broad population using simple criteria.
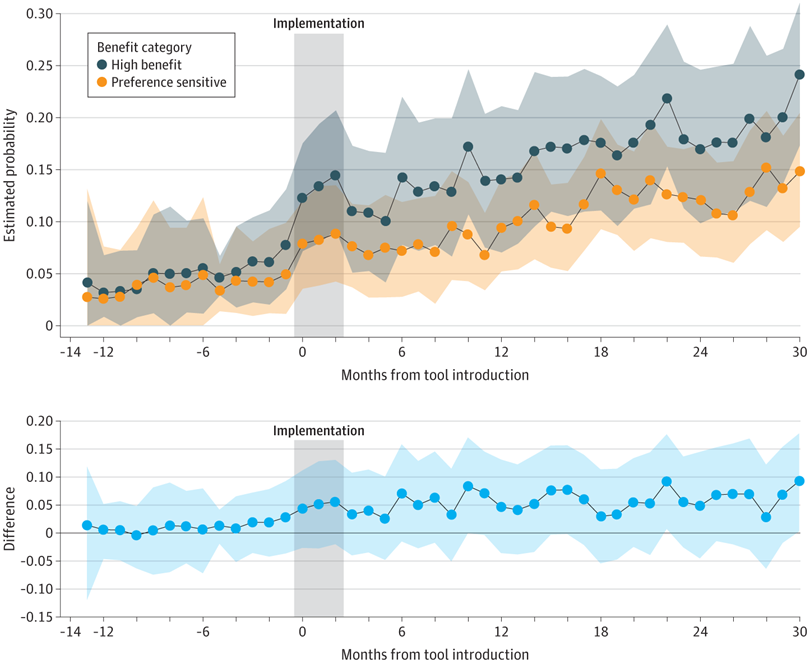
Click to Enlarge: Predicted Probability of Uptake of Low-Dose Computed Tomography Lung Cancer Screening by Month. Shaded areas indicate 95% CIs (calculated by running a simulation 100 000 times).
Source: JAMA Network Open
In the new study, VA researchers examined screening uptake following implementation of a shared decision-making (SDM) tool that alerts clinicians to encourage screening more strongly for patients predicted to be at high benefit. The study was conducted at six VA sites that used a standard set of clinical reminders to prompt primary care clinicians and screening coordinators to engage in SDM for LCS-eligible persons. Participants were persons without a history of LCS who met LCS eligibility criteria at the time (aged 55–80 years, smoked ≥30 pack-years and current smoking or quit <15 years ago) and were not documented to be an inappropriate candidate for LCS by a clinician during October 2017 through September 2019. Data were analyzed from September to November 2023.1
The study cohort included 9,904 patients, of whom 1,084 (11%) received screening. Based on their combination of risk factors, 5,153 patients (52%) were predicted to be at intermediate benefit and, 4751 (48%) were at high benefit. The likelihood of being screened increased over time, indicating a mean 6% increase in LCS uptake per month during the study, and the odds of screening were lower in those with an estimated life expectancy of less than 10 years. The association between predicted benefit to LCS uptake was greater after tool implementation; that is, more benefit-based LCS. This association was sustained, and, by the final month of the study, the mean estimated probability of getting screened for a high-benefit person was 24.8% for a person at intermediate benefit.
Finally, to look for unintended consequences of tool implementation, the researchers examined the rate of potential low-value LCS uptake (screening when ineligible by U.S. Preventive Services Task Force criteria and not high-benefit by prediction) during each study period. Low-value LCS uptake was low during all time periods in this cohort and appeared to decrease, if anything, after tool implementation, the researchers stated.
Improved Uptake
“Our quasi-experimental findings suggest that implementing a robust approach to personalized LCS, which integrates SDM and a decision support tool augmented by a prediction model, is associated with improved screening uptake and may be particularly important for those most likely to benefit,” the authors wrote in JAMA Network Open. “The sustained, higher rate of uptake among high-benefit persons in this study reflects the tool’s emphasis on identifying high-benefit persons for stronger encouragement to get screened.”
Importantly, the increased uptake among high benefit persons did not come at the cost of reducing uptakes among eligible persons at intermediate benefit—for whom screening is still appropriate if aligned with the patient’s personal preference—the researchers wrote. “Meanwhile, after tool implementation, there were substantially lower odds of LCS among people with less than 10 years of life expectancy, suggesting the tool’s ability to also reduce low-value screening. These findings are highly aligned with how the decision tool was designed,” they wrote.
“We found that, following implementation of a robust approach to personalized SDM for LCS, people with higher anticipated benefit from LCS had a greater increase in screening uptake than those with intermediate benefit,” the researchers concluded. “This quasi-experimental finding supports the use of prediction to optimize the delivery of LCS. A cluster-randomized or stepped-wedge randomized trial testing the feasibility of implementing prediction-augmented LCS across diverse health systems is needed to further assess the scalability of this approach.”
- Caverly, T. J., Wiener, R. S., Kumbier, K., Lowery, J., & Fagerlin, A. (2024). Prediction-Augmented Shared Decision-Making and Lung Cancer Screening Uptake. JAMA Network Open, 7(7), e2419624. https://doi.org/10.1001/jamanetworkopen.2024.19624

