Click to Enlarge: Univariable and Multivariable Models for HCC Development With Liver Transplantation and Death as Competing Events Source: JAMA Network Open
LOS ANGELES — U.S. veterans are much more likely to be diagnosed with hepatocellular carcinoma, but at least one toxic exposure during military service doesn’t appear to have much to do with that.
Hepatocellular carcinoma (HCC) and related mortality are on the rise, but the cause does not appear to be Agent Orange exposure with veterans from the Vietnam era.
“Viral hepatitis and alcohol are leading risk factors; however, other risk factors among veterans are less defined, including Agent Orange (AO), an herbicide linked to several cancers,” wrote researchers from the VA Greater Los Angeles Healthcare System,
David Geffen School of Medicine at the University of California, Los Angeles, and colleagues.
The study team assessed the association of AO exposure and HCC in a national cohort of Vietnam veterans. Results were reported in JAMA Network Open.1
The retrospective cohort study included Vietnam veterans who served between 1966 and 1975, were male, were older than 18 years at the time of deployment and had established follow-up in the VA healthcare system between 2000 and 2019.
Researchers identified veterans with AO exposure from the disability data via validated clinical surveys. They also collected relevant clinical risk factors for cirrhosis and HCC.
U.S. veterans are estimated to be five times more likely to develop HCC than the general population. In 2021, 2,000 veterans in VA care were diagnosed with HCC, and the incidence at the VA has increased significantly over the past 20 years, mainly due to the rise in cirrhosis
For the study, patients were stratified based on cirrhosis status, as defined by consecutive diagnosis found by documented International Classification of Diseases, Ninth Revision and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision scores or calculated Fibrosis-4 scores. Data were collected from Jan. 1, 2019, to Dec. 31, 2020, and analyzed from December 2020 to October 2023.
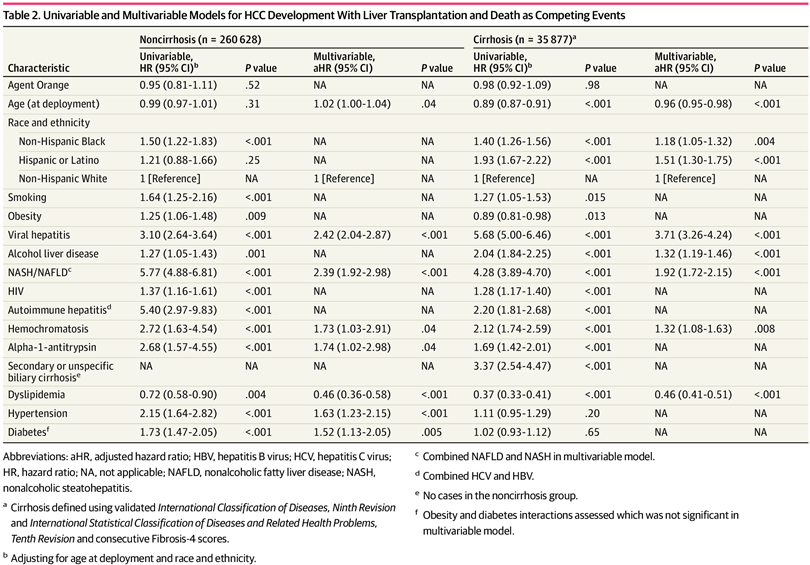
Incident HCC was defined as the primary outcome. AO and HCC association was estimated using a multivariable Cox regression analysis, with death and liver transplant as competing events, the authors explained.
Of the 296,505 eligible veterans, 75.1% were white and 15.0% were Black. Of those, 57% had AO exposure at a median age of 21.62. The rate of cirrhosis was 13.1% among those not exposed to AO, compared to 11.3% of those who had.
Veterans who were not exposed to AO were more likely to smoke (109 689 of 126 413 [86.8%] vs 146 061 of 170 090 [85.9%]); use alcohol (54 147 of 126 413 [42.8%] vs 71 951 of 170 090 [42.3%]) and have viral hepatitis (47 722 of 126 413 [37.8%] vs 58 942 of 170 090 [34.7%]).
“In a multivariable competing risk model, AO exposure was not associated with HCC,” the researchers pointed out. “Among veterans with cirrhosis, self-identification as Hispanic individuals (aHR, 1.51; 95% CI, 1.30-1.75; P <.001) or Black individuals (aHR, 1.18; 95% CI, 1.05-1.32; P = .004), and having a diagnosis of viral hepatitis (aHR, 3.71; 95% CI, 3.26-4.24; P <.001), alcohol-associated liver disease (aHR, 1.32; 95% CI, 1.19-1.46; P <.001), and nonalcoholic fatty liver disease (NAFLD) (aHR, 1.92; 95% CI, 1.72-2.15; P <.001) were associated with HCC.”
Among veterans without cirrhosis, meanwhile, hypertension (aHR, 1.63; 95% CI, 1.23-2.15; P <.001) and diabetes (aHR, 1.52; 95% CI, 1.13-2.05; P = .005) were also associated with HCC. “Early smoking and alcohol use were significant risk factors for HCC,” the study authors advised.
The study team concluded, based on the large nationwide cohort study of Vietnam veterans, that AO exposure was not associated with HCC, explaining, “Smoking, alcohol, viral hepatitis, and NAFLD were the most important clinical risk factors for HCC.”
- Benhammou JN, Leng M, Shah SC, Cholankeril G, Dong TS, Patel AA, Tong MJ. Exposure to Agent Orange and Hepatocellular Carcinoma Among US Military Personnel. JAMA Netw Open. 2023 Dec 1;6(12):e2346380. doi: 10.1001/jamanetworkopen.2023.46380. PMID: 38048128; PMCID: PMC10696483.


