Patients with serious mental illnesses (SMI) such as schizophrenia or bipolar disorder are socially isolated. That was assumed to be the cause of social cognitive deficits and high social avoidance motivation in the cohorts. A recent VA study found, however, that those are actually symptoms of the SMI and not the result of living conditions.
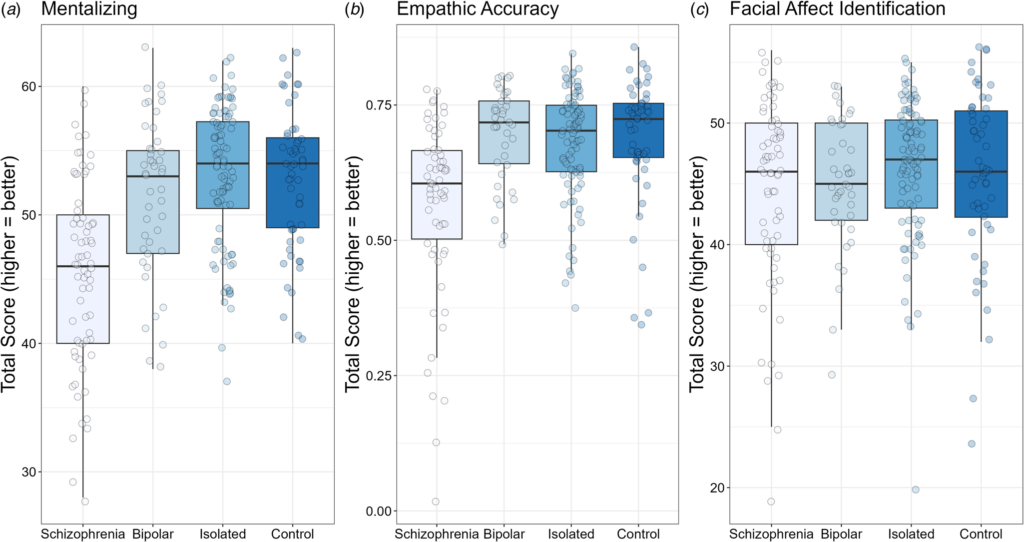
Click to Enlarge: Box plots for mentalizing (TASIT; Panel A), empathic accuracy (Panel B), and facial affect identification (Panel C). For all tasks, higher scores indicate better performance. Solid black horizontal line indicates the median. Each dot represents the score for an individual within that group. Source: Psychological Medicine
LOS ANGELES — While individuals with schizophrenia and bipolar disorder often have difficulty with relationships and being part of a community, a recent study involving U.S. veterans has found that social cognitive deficits and high social avoidance motivation appear to be actual features of the clinical conditions and not the result of living in social isolation.
The study published in Psychological Medicine investigated whether social cognition or social motivation impairments are linked to mental health disorders (schizophrenia or bipolar disorder) or to being socially isolated.1
Study authors were affiliated with VA Greater Los Angeles, CA, Healthcare System and VA Rehabilitation R&D Center on Enhancing Community Integration for Homeless Veterans in Los Angeles.
Based on VA data on serious mental illness, which includes schizophrenia and bipolar disorder, as of the first quarter of fiscal year 2024, the researchers reported that, in the past 12 months across the nation, 224,232 veterans were diagnosed with serious mental illness as diagnosed by VA National Psychosis Registry criteria.
On average, people with schizophrenia are “more socially isolated, lonelier, have more social cognitive impairment, and are less socially motivated than healthy individuals.” Individuals with bipolar disorder also have social isolation, but typically less than what is seen in schizophrenia. Social isolation is defined as “the objective lack of peer and family relationships and minimal participation in community activities,” according to the article.
“Social cognition and social motivation are important determinants of social integration in people with schizophrenia,” Michael F. Green, Ph.D., director of the VA Rehabilitation R&D Center on Enhancing Community Integration for Homeless Veterans, told the Compendium of Federal Medicine. “In other words, deficits in these areas predict the level of social functioning. However, since people with schizophrenia and bipolar disorder often are socially isolated, we do not know whether the deficits are due to that isolation or a core part of the conditions.”
The study compared four groups of subjects on loneliness, social cognition, approach and avoidance social motivation. One group had a diagnosis of schizophrenia (72 outpatients), and another had a diagnosis of bipolar disorder (48 outpatients). Most of the participants were part of a registry kept at the VA, and not all were veterans. The other two groups consisted of people from the community (151 individuals). One group self-reported being socially isolated, and another group was socially connected.
The clinical groups were recruited from outpatient clinics at the VA Greater Los Angeles Healthcare System and the University of California, Los Angeles (UCLA), and outpatient board and care facilities in the Los Angeles area. Psychiatric diagnoses were established with the Structured Clinical Interview for DSM-5 (SCID-5) from Modules A-E and the PTSD section, and medical records were examined to validate information from interviews when they were available.
All clinical participants were stable “with no hospitalizations within three months and no changes in psychoactive medication type/dosage within four weeks,” according to the study. Patients in both the schizophrenia and bipolar disorder patient groups were receiving psychoactive medications at the time of assessment.
All community participants provided psychiatric history through the SCID-5 and select sections of the SCID for Personality Disorders (SCID-PD) assessing avoidant, paranoid, schizoid, schizotypal and borderline characteristics. They were excluded if they met criteria for a lifetime history of a psychotic disorder or bipolar disorder, the authors explained.
The participants were 20 to 60 years old and had a sufficient understanding of English, no clinically significant neurological disease (e.g., epilepsy), no history of a serious head injury, no use of sedatives or benzodiazepines within 12 hours of testing, no evidence of IQ less than 70 or developmental disability based on the Wide-Range Achievement Test 3rd ed. reading subtest, no substance-use disorder at moderate level or greater in the past three months and no current mood episode that met clinical criteria for depression, hypomania or mania, the researchers explained.
“The results suggest that social cognitive deficits in schizophrenia, and high social avoidance motivation in both schizophrenia and bipolar disorder, are distinct features of the clinical conditions and are not simply a result of living lives of social isolation,” Green said. “In contrast, loneliness and social approach motivation appears to be more related to one’s level of social isolation.”
The study found that “individuals with schizophrenia (n = 72) showed intermediate levels of social isolation, loneliness, and social approach motivation between the isolated (n = 96) and connected control (n = 55) groups.” However, schizophrenia patients “showed significant deficits in social cognition compared to both community groups.”
In addition, the authors discovered that “individuals with bipolar disorder (n = 48) were intermediate between isolated and control groups for loneliness and social approach.” The individuals with bipolar disorder “did not show deficits on social cognition tasks, and both clinical groups (patients with schizophrenia or bipolar disorder) had higher social avoidance than both community groups.”
“Because social cognition for schizophrenia and social avoidance for both schizophrenia and bipolar disorder are directly tied to the clinical conditions, they are good targets for intervention to improve social integration among veterans with these conditions,” Green recommended to healthcare professionals. “These results reinforce the idea that a careful consideration of social and interpersonal context should be an important part of the treatment for these conditions.”
- Green MF, Wynn JK, Eisenberger NI, et al. Social cognition and social motivation in schizophrenia and bipolar disorder: are impairments linked to the disorder or to being socially isolated? Psychological Medicine. Published online 2024:1-9. doi:10.1017/S0033291724000102


