Often Suffer More Medical Morbidity With Aging
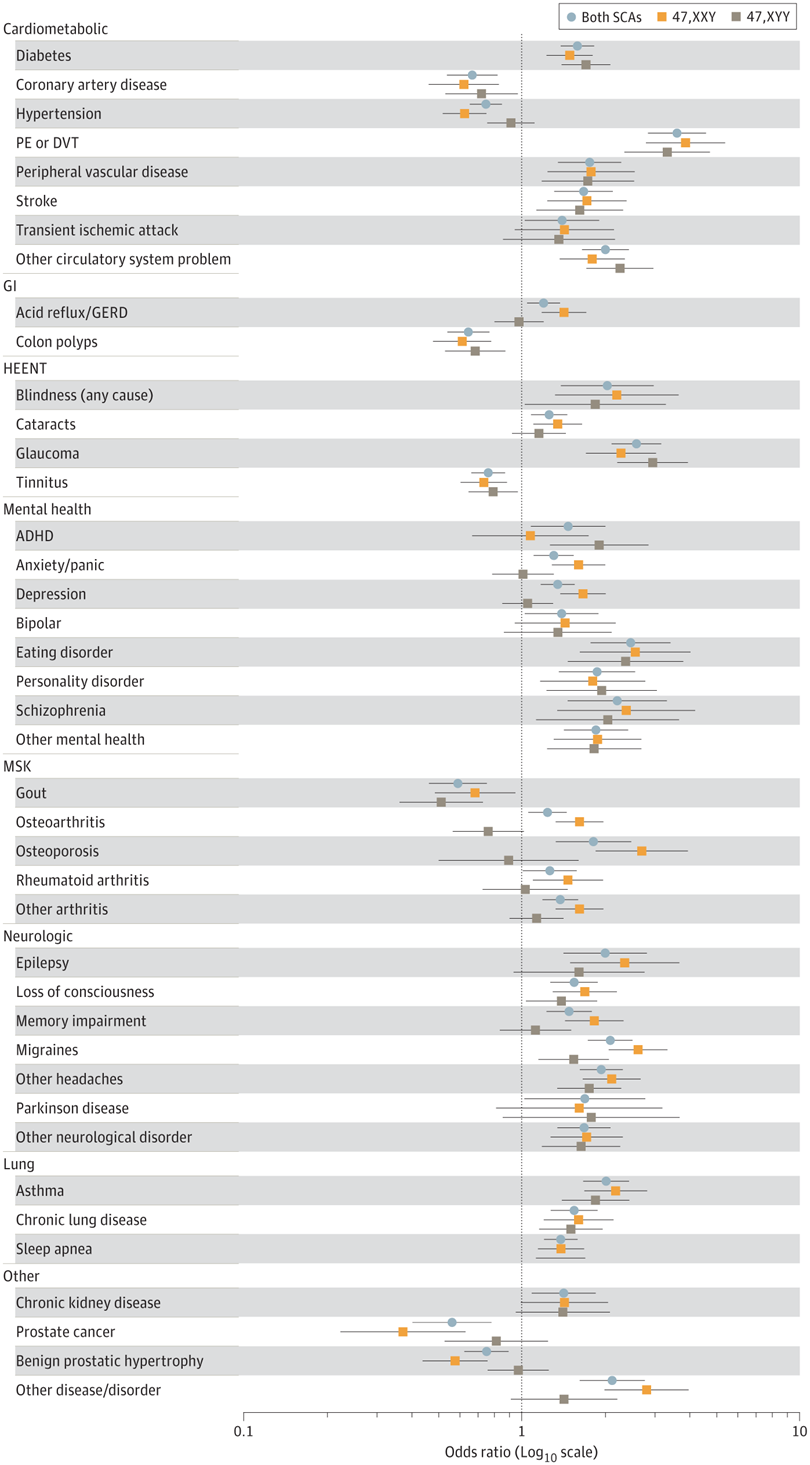
Click to Enlarge: Odds of self-reported diagnoses are presented compared with their respective matched controls from the baseline survey. Point estimates are the odds ratios (OR) with odds greater than 1 representing higher odds in SCA; error bars represent the 95% CIs. Only conditions statistically different between SCA and controls and with a minimum of 10 individuals are included. ADHD indicates attention deficit/hyperactivity disorder; DVT, deep venous thrombosis; GERD, gastroesophageal reflux disease; GI, gastrointestinal; HEENT, head, eyes, ears, nose, throat; MSK, musculoskeletal; PE, pulmonary embolus. Source: JAMA Network Open
SAN DIEGO — Men with sex chromosome aneuploidies, meaning they have an additional X or Y chromosome, successfully serve in the U.S. military, but they have been greatly underdiagnosed and have higher medical morbidity with aging, according to a recent study.
The cross-sectional study published recently in JAMA Network Open investigated the prevalence of an additional X or Y chromosome among men who served in the U.S. military and the morbidity outcomes associated with these conditions.1
Study authors, including those affiliated with VA Healthcare Systems in San Diego, Salt Lake City and Boston, examined health outcomes in 140,000 male veterans who were enrolled in the Million Veteran Program, a national VA research program on genes and health. A major goal of the Million Veteran Program is to determine the role of testosterone in health outcomes, according to the authors.
“When we completed our genome-wide association study and phenome-wide association study analyses of morning testosterone levels in ~140,000 male veterans with European, African, East Asian or Admixed American ancestry, we discovered novel, ancestry-specific gene variants that regulate testosterone and provide disease risk stratification for metabolic, hepatic and other medical illnesses,” Richard L. Hauger, MD, a Million Veteran Program researcher and psychiatrist at the VA San Diego Health Care System, told U.S. Medicine.
“Surprisingly, our testosterone genetic research identified 862 men with Klinefelter syndrome (47,XXY), which is the most prevalent genetic cause of hypogonadism, and 747 men with 47,XYY. This unexpected finding was the genesis of our sex chromosome aneuploidy research, which is the largest, multi-ancestry study of men with 47,XXY or 47,XYY in an aging population,” said Hauger, who also is a professor at the Center for Behavior Genetics of Aging at the University of California, San Diego School of Medicine.
Sex chromosomal aneuploidy is caused by random errors in meiosis (cell division for generating sperm and eggs for sexual reproduction) and is assumed to be independent of genetic or social constructs, he explained.
“The reported phenotypes of men with 47,XXY and 47,XYY syndromes include tall stature, multisystem comorbidities, and poor health-related quality of life, but knowledge about these sex chromosome aneuploidy conditions has been derived from studies in the less than 15% of patients who are clinically diagnosed and also lack diversity in age and genetic ancestry,” the authors reported.
This study found “the estimates for prevalence of sex chromosome aneuploidies in male veterans are 145/100,000 (1 in 690) men for 47,XXY and 125/100,000 (1 in 800) men for 47,XYY,” Hauger said.
“These estimates are within the expected range for reported prevalence in other studies, which are 103-174/100,000 men for 47,XXY and 69-98/100,000 men for 47,XYY,” Hauger added. “While the veteran men with 47,XXY or 47,XYY included in the study had successfully served in the military earlier in their life, they experienced higher morbidity and worse quality of life during aging.”
“Based on the results of our study, men with either 47,XXY or 47,XYY successfully completed military duty with service records very similar to men without sex chromosome aneuploidy (46,XY),” Hauger said. “Men with sex chromosome aneuploidy, however, exhibited higher medical morbidity with greater incidence of diabetes, peripheral vascular disease, glaucoma, affective illness and other major clinical disorders as well as poor quality of life during aging.”
Genetic characteristics also play a role in sex chromosome aneuploidies, the authors pointed out.
“We discovered that the estimated prevalence of sex chromosome aneuploidy was over twice as high in men with European or East Asian ancestry compared to men with African or Hispanic ancestry,” Hauger said. “We are currently investigating mechanisms that mediate these ancestry-specific differences in prevalence of 47,XXY and 47,XYY.”
Similar in Women, Men
However, sex chromosome aneuploidies aren’t more common in men than women. The incidence of 47,XXX in women is about 1:1000, which is fairly similar to the incidence of 47,XXY and 47,XYY in men, according to the authors.
Sex chromosome aneuploidies are underdiagnosed because the “U.S. military and the VAHS don’t routinely conduct genetic analyses, such as sex chromosome dosage by gene microarray intensity measurements,” Hauger explained.
“To our knowledge, our study is the first to compare morbidity, healthcare utilization, and quality of life between men with 47,XXY and without a clinical diagnosis of Klinefelter syndrome,” Hauger said. “Interestingly, men with 47,XXY with a clinical diagnosis of Klinefelter syndrome had lower medical comorbidity than those undiagnosed.”
The study found that “only 26.2% of men with 47,XXY in this study population had a diagnosis of Klinefelter syndrome with clinical ascertainment, while only 0.3% of men with 47,XYY had a clinical diagnosis,” the authors reported.
“Importantly, medical comorbidity was significantly lower in men with 47,XXY with a clinical diagnosis of Klinefelter syndrome compared to those without a diagnosis. This suggests that a clinical diagnosis of sex chromosome aneuploidy may reduce comorbidity burden,” Hauger said.
The study’s results suggest the VAHS should consider screening men with hypogonadism for 47,XXY. VA urologists could also consider genetic screening for Klinefelter Syndrome for veterans that present with oligospermia, azoospermia and other testicular dysfunctions, according to the report.
“Our study also suggests that veterans with Klinefelter syndrome can benefit from closer primary care and medical specialty follow-up with more preventive medicine interventions that can reduce medical comorbidity resulting from 47,XXY,” Hauger said.
The Million Veteran Program research is generating critical information about genetic diversity of men and women across multiple ancestries. Knowledge and understanding of genetic diversity derived from this research will help to transform VA clinical care by leading development of genetically informed therapeutic interventions to target and maximize effective clinical care ensuring the best health outcomes, Hauger explained.
“Based on our study results, we propose that men with 47,XXY or 47,XYY receive regular clinical follow-up to monitor for cardiovascular disease, diabetes, thrombotic disorders, glaucoma and other medical disorders that have higher incidence in men with sex chromosome aneuploidy,” Hauger said.
“Partnership between the MVP [Million Veteran Program] and VA clinical operations will hopefully ensure that genetic and genomic insights into human illnesses generated by MVP are translated with appropriate clinical validation into improving precision care of all veterans throughout the VA Healthcare System,” Hauger added.
- Davis SM, Teerlink C, Lynch JA, et al. Prevalence, Morbidity, and Mortality of Men With Sex Chromosome Aneuploidy in the Million Veteran Program Cohort. JAMA Netw Open. 2024;7(3):e244113. doi:10.1001/jamanetworkopen.2024.4113

