Questions Raised About Longer Term GLP-1RA Benefits
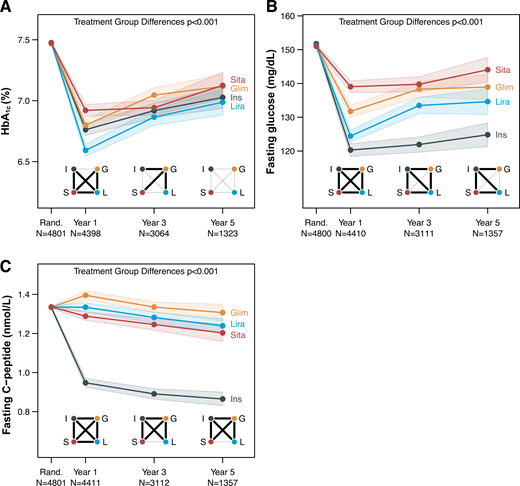
Click to Enlarge: Effects of four different glucose-lowering medications on levels of HbA1c (A), fasting glucose (B), and fasting C-peptide (C). The square diagrams in the lower part of the panels denote the range of the P values for the six pairwise group comparisons of treatment groups. Bold line represents P < 0.05. G and Glim, glimepiride; I and Ins, insulin glargine; L and Lira, liraglutide; and S and Sita, sitagliptin. Rand. represents randomization, or baseline. Source: Diabetes Care
AURORA, CO — For the estimated 1 in 10 Americans—or 1 in 4 veterans—with Type 2 diabetes, keeping blood glucose levels in the near-normal range reduces the risk of complications such as heart, kidney and eye disease. But maintaining long-term glycemic control can be a challenging process due to a number of factors, one of the most important of which is the progressive loss—5-10% per year—of β-cell function, according to new research.
“The sensitivity to insulin action and insulin secretion from the pancreas’ β -cells are known to be important contributors to Type 2 diabetes,” said Neda Rasouli, MD, professor of medicine in the Division of Endocrinology, Metabolism and Diabetes at the University of Colorado and investigator at the VA Eastern Colorado Health Care System, “Therefore, identifying effective interventions to delay or prevent this deterioration is of great value.”
Rasouli was the lead author of the new study examining the effect of four commonly used glucose-lowering medications on insulin sensitivity, β-cell responses and β-cell function.1
The study, published in Diabetes Care, is a secondary analysis of data from the Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness (GRADE) Study. GRADE, which included more than 5,000 volunteer participants with Type 2 diabetes. Including diverse racial and ethnic groups, the trial was conducted at 36 US medical centers, including 10 VA centers and 9 subsites between 2013 and 2021. It was designed to compare insulin glargine, liraglutide, glimepiride, and sitagliptin, four major medications approved by the Food and Drug Administration, to treat diabetes in combination with metformin, the usual first-line drug.1,2
Major results of the original study focused on the relative differences in blood glucose levels and the occurrence of cardiovascular outcomes, like heart attacks and stroke, were published in two papers in The New England Journal of Medicine in September 2022, Rasouli said.
The new study used Homeostasis Model Assessment 2 (HOMA2), an updated and improved version of the original HOMA model, to estimate insulin sensitivity and fasting β-cell function at baseline and 1, 3 and 5 years on treatment. Oral glucose tolerance test β-cell responses (C-peptide index [CPI] and total C-peptide response) were evaluated at the same time points.
The most important finding overall, “which is unfortunately not positive,” Rasouli said, “is the observation that none of these glucose-lowering medications were able to halt the progressive loss of β-cell function and glycemic deterioration over time in people with Type 2 diabetes. The loss of insulin secretion was critically related to the progressive worsening of blood sugar control with all four medications, with reduced insulin sensitivity contributing to the outcomes of treatment.”
A more specific finding, she said, was that “while liraglutide did result in a robust enhancement of the β-cell response and insulin secretion in the short term—after 1 year of treatment—we also noted a sharper decline in β-cell function with liraglutide, compared to other treatment groups after year 1.” This suggests that the beneficial effects of liraglutide may not be durable and that the results of short-term studies cannot be extrapolated to long-term effects, Rasouli explained.
Liraglutide Finding Surprising
This finding concerning liraglutide was surprising, considering it is a member of the glucagon-like peptide-1 receptor agonists (GLP-1RA) class of drugs, Rasouli said. Medications in the GLP-1RA class, which mimic the action of the natural hormone GLP-1 that plays a key role in glucose metabolism, were previously believed to have a positive effect on β -cell function, as reported in short-term studies. “However, GRADE showed us that the long-term effects are not as positive and promising as initially thought.”
Also surprising, she said, was the favorable effect of sitagliptin on the early insulin response to IV glucose, as measured using the C-peptide index. C-peptide, a byproduct of insulin production, serves as a useful marker for evaluating endogenous insulin secretion. “Although the combination therapy of sitagliptin and metformin proved to be the least effective in maintaining glycemic control at target, the sitagliptin group exhibited a very similar improvement in early insulin secretion compared to liraglutide, which was unexpected.”
Rasouli said the utility of measures of insulin sensitivity and β-cell function in clinical practice is still a subject of debate. “However, we are all moving toward precision medicine and investigating factors that might predict a better response to certain medications, or studying the course of diabetes and its complications in people with different subtypes of diabetes based on their measures of insulin sensitivity and β-cell function.”
“Diabetes is a progressive disease associated with numerous complications that are irreversible,” she continued. “Adopting a holistic approach to diabetes management is crucial, involving personalized targets for glycemic control and engaging the patient in decision-making processes. Early and aggressive intervention is essential to prevent long-term complications. There remains a pressing need for interventions that can preserve β -cell function to sustain long-term glycemic control.”
- Rasouli, N., Younes, N., Ghosh, A., Albu, J., et al. (2024). Longitudinal Effects of Glucose-Lowering Medications on β-Cell Responses and Insulin Sensitivity in Type 2 Diabetes: The GRADE Randomized Clinical Trial. Diabetes Care, 47(4), 580–588. https://doi.org/10.2337/dc23-1070
- GRADE Study Research Group; Nathan DM, Lachin JM, Balasubramanyam A, Burch HB, et. Al. Glycemia Reduction in Type 2 Diabetes – Glycemic Outcomes. N Engl J Med. 2022 Sep 22;387(12):1063-1074. doi: 10.1056/NEJMoa2200433. PMID: 36129996; PMCID: PMC9829320.


