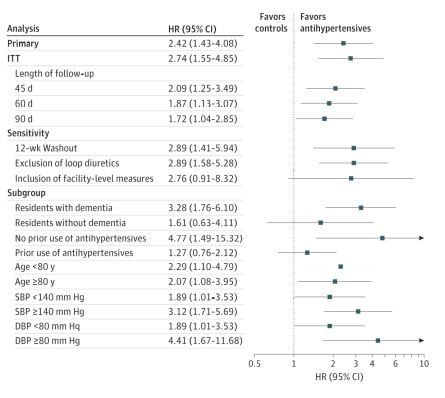
Click to Enlarge: Adjusted Risk of Fracture Among Nursing Home Residents Initiating Antihypertensive Medication: Sensitivity and Subgroup Analyses
Analyses were adjusted using 1:4 propensity score matching for baseline covariates, described in Table 2. For all subgroup analyses, the propensity scores were re-estimated and the cohorts were rematched. DBP indicates diastolic blood pressure; HR, hazard ratio; ITT, intention to treat, and SBP, systolic blood pressure. Source: JAMA Network Open
EAST ORANGE, NJ — Starting an antihypertensive treatment is associated with a significant increase in fracture risk in older long-term VHA nursing home residents, according to a recent study.
The retrospective cohort study published in JAMA Internal Medicine examined the association between initiation of an antihypertensive medication and its correlation with fracture risk among older nursing home veterans.1
The study authors are affiliated with VA New Jersey Health Care System in East Orange, NJ; VA Palo Alto, CA, Healthcare System; and the San Francisco VAMC.
It was important to explore this topic, because “limited evidence exists on the association between initiation of antihypertensive medication and risk of fractures in older long-term nursing home residents,” study authors wrote.
Researchers used target trial emulation for data from 29,648 older long-term care nursing home residents in the VHA from Jan. 1, 2006, to Oct. 31, 2019. Data were analyzed from Dec. 1, 2021, to Nov. 11, 2023. The authors identified episodes of antihypertensive medication initiation, and eligible initiation episodes were matched with comparable controls who did not initiate therapy, the authors explained.
“Treatment initiation was defined as an increase in the number of blood pressure-lowering medication classes compared with the prior four weeks (i.e., therapy augmentation), and instances of switching were excluded,” they explained. “Patients initiating their first antihypertensive medication (i.e., not receiving any prior treatment in the preceding four weeks) were also included. The date of medication initiation was indicated as the index date for the exposure group.”
Patients in the cohort group “needed to be at least 65 years old, have no evidence of end-stage kidney disease in the preceding year, and have at least one documented measurement of systolic and diastolic blood pressure within two weeks of the index date. With multiple blood pressure assessments, the most recent value prior to the index date was used. Patients were required to maintain a stable antihypertensive treatment regimen for four consecutive weeks prior to the index date (i.e., date of medication initiation), meaning there weren’t any changes in the number of antihypertensive drug classes in each of the preceding four weeks. The cohort was restricted to patients with at least 90 days of nursing home stay, and medication use was measured starting from the 91st day,” the authors pointed out.
For patients in the control group, each week of the nursing home stay was assessed by evaluating whether the eligibility criteria were met (i.e., stable regimen, documented blood pressure and no end-stage kidney disease).
“We found that starting an antihypertensive treatment was associated with a significant increase in fracture risk,” lead author Chintan Dave, PharmD, PhD, a statistician with the VA New Jersey Health Care System in New Brunswick, told U.S. Medicine. “More specifically, the incidence rate of fractures per 100 person-years was 5.4 in residents who began antihypertensive therapy, compared to 2.2 in those who did not, which corresponded to an adjusted hazard ratio of 2.42 (95% CI, 1.43-4.08).”
In the study, the primary outcome was nontraumatic fracture of the humerus, hip, pelvis, radius or ulna within 30 days of antihypertensive medication initiation. The researchers calculated results among subgroups of residents with dementia, across systolic blood pressure thresholds of 140 mm Hg and diastolic blood pressure thresholds of 80 mm Hg and with use of prior antihypertensive therapies. Analyses were adjusted for more than 50 baseline covariates using 1:4 propensity score matching, according to the authors.
Who’s Most at Risk?
“The most critical finding from our study for healthcare professionals is the notable increase in fracture risk following the initiation of antihypertensive medications in older nursing home residents,” Dave said. “This risk was even more pronounced among specific groups, such as those with dementia, higher baseline blood pressures and residents who were not recently on any antihypertensive.”
The study team pointed out that risk was “numerically higher in subgroups of residents with dementia or with systolic blood pressure of 140 mm Hg or higher or diastolic blood pressure of 80 mm Hg or higher.” Based on the study’s findings and, given the increased risk of fractures associated with initiating antihypertensive medications, the authors advised that healthcare professionals use “caution and additional monitoring when initiating antihypertensive medication in this vulnerable population.”
The study authors recommended that healthcare professionals take three crucial actions. First, it’s important to “assess individual risk. Before initiating treatment, evaluate each patient’s risk factors for falls and fractures, including their cognitive status and previous fall history,” Dave explained.
Second, it’s key to “monitor patients closely. After starting antihypertensive therapy, healthcare professionals need to closely monitor patients for signs of adverse effects such as dizziness or unsteadiness, which can predispose them to falls,” he continued.
Lastly, it’s critical to “adjust treatment as necessary. Be prepared to adjust dosages or switch medications if patients experience adverse effects,” Dave added.
The study’s results have important clinical implications. “The incidence of fall-related mortality has trended upward in the United States, nearly doubling from 2000 to 2013, from 29.6 to 56.7 deaths per 100,000 adults,” according to the report, which added that falls are the primary contributor to fractures and are associated with an increase in overall mortality. In older nursing home residents, “hip fractures alone have been linked to one-year mortality rates exceeding 40%.”
In this study, the “observed excess rates of fracture per 100-person years due to antihypertensive medication initiation were high and ranged between 3.1 for the overall cohort and approaching 5.0 among certain vulnerable subgroups (e.g., residents with dementia),” according to the authors.
Despite existing preventive measures that nursing homes have taken to prevent falls and fractures, patients in facilities initiating antihypertensive medication had a higher risk of fractures and falls. In this population, fracture prevention is crucial, and “commonly prescribed medications, such as antihypertensive medications, represent a prominent modifiable risk factor,” the study emphasized.
In older nursing home residents, a comprehensive group of factors should “guide the choice of antihypertensive medication, including the patient’s complete medical history, specific clinical indication for treatment and potential for adverse reactions,” the study concluded, noting that the factors should also “contextualize a limited life expectancy against the anticipated time horizon over which the cardiovascular benefits are likely to manifest.”
- Dave CV, Li Y, Steinman MA, Lee SJ, et. Al. Antihypertensive Medication and Fracture Risk in Older Veterans Health Administration Nursing Home Residents. JAMA Intern Med. 2024 Apr 22:e240507. doi: 10.1001/jamainternmed.2024.0507. Epub ahead of print. PMID: 38648065; PMCID: PMC11036308.

