Older Patients Appear to Be Most Affected
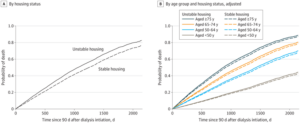
A, Cumulative incidence of deaths among veterans by housing status. B, Cumulative incidence of deaths among veterans by age group and housing status. Data in panels A and B were adjusted for sex, race and ethnicity, year of dialysis initiation, predialysis nephrology care, incident dialysis modality, cause of kidney failure, incident vascular access, primary insurance, urban or rural residence, and comorbidities. Data in panel A were additionally adjusted for age, age-squared, and age × unstable housing. Curves are based on a median age of 68 years, year 2014, and the most common value for all other covariates.
AUSTIN, TX—Unstable housing appears to contribute to socioeconomic disparities in mortality among U.S. veterans receiving dialysis, with older adults being especially vulnerable, according to a new study.
The study team led by the University of Texas at Austin Dell Medical School and with participation from the Audie L. Murphy VAMC in San Antonio and the Alabama Veterans Affairs Healthcare System in Birmingham performed a cohort study of 25,689 veterans receiving dialysis. It concluded that unstable housing was associated with an increased risk of all-cause mortality and that danger increased with age, veterans aged 75 to 85 years having the highest risk.
“Housing status is an important health determinant, yet little is known about unstable housing among individuals receiving dialysis,” the researchers wrote in JAMA Network Open.1
Data from the VHA and the U.S. Renal Data System for patients who initiated dialysis between Oct. 1, 2012, and Dec. 31, 2018, was included in the study. The focus was on 25,689 veterans who used VHA outpatient services and completed one or more unstable housing screenings within a three-year period before starting dialysis. Data analysis was conducted from Jan. 24 to June 16, 2023.
For the purposes of the study, unstable housing was defined as self-report of not having stable housing within the past two months or having concerns about stable housing in the next two months. Defined as the primary outcome was all-cause mortality.
Participants had a median age of 68 (IQR, 62-74) years; most were men (98%), and more than half (52%) were white. Of those, 771 veterans (3%) had a positive screen for unstable housing within a three-year period before starting dialysis.
“Compared with veterans with stable housing, those with unstable housing were younger (mean [SD] age, 61 [8] vs. 68 [10] years), were more likely to be Black (45% vs 32%) or Hispanic (9% vs 7%), and were more likely to start dialysis with a central venous catheter (77% vs 66%), receive in-center hemodialysis (96% vs 91%), and have non-Medicare insurance (53% vs 28%),” the study advised.
Factors associated with unstable housing included:
- Hispanic ethnicity,
- non-arteriovenous fistula vascular access,
- lack of predialysis nephrology care, and
- non-Medicare insurance.
“Veterans with unstable housing had higher all-cause mortality (adjusted hazard ratio [AHR], 1.20 [95% CI, 1.04 to 1.37] for a median age of 68 years), and risks increased with age (P = .01 for interaction),” the authors pointed out. “In age-stratified analyses, unstable housing was associated with higher mortality among veterans aged 75 to 85 years (AHR, 1.64 [95% CI, 1.18 to 2.28]), but associations were not observed for other age groups.”
The researchers called for increased efforts to understand the experiences of older adults with unstable housing and how that affects patients receiving dialysis.
Homelessness Included
Background information in the article noted that unstable housing is variably defined but includes homelessness and housing that might be lost if it is unaffordable, overcrowded or dangerous. “There is mounting concern that housing issues may be prominent among individuals receiving dialysis, given increasing housing costs across the U.S. and the job loss and financial resource strain associated with dialysis initiation,” the authors suggested. “Unstable housing has the potential to negatively affect nearly every aspect of dialysis care and increase complications, and it limits access to home dialysis modalities and kidney transplantation. Interventions addressing housing as part of clinical care have the potential to lower risk of mortality. However, little is known about unstable housing among individuals receiving dialysis.”
They add that screening for unstable housing at VHA clinics began in 2012 as part of national efforts to limit the detrimental effect of uncertain housing. Any positive screen for unstable housing triggers a timely referral to veteran-specific housing programs, according to the researchers, who pointed out that, with that initiative, the number of homeless veterans decreased from 74 087 to 33 129 between 2010 and 2022.
That’s important, they emphasized, because even in the general population, unstable housing is thought to affect outcomes because of the difficulties in seeking and obtaining healthcare. “When individuals experience unstable housing, their housing may be prioritized over their health,” according to the report. “High housing costs limit the availability of money for food, medications, and transportation. Limited financial resources may contribute to difficulty in scheduling and attending nephrology appointments or obtaining arteriovenous fistulas placed for individuals with advanced chronic kidney disease. The demands associated with dialysis may limit patients’ ability to work, further limiting financial resources, and increasing stress. Stress is postulated to enhance activation of the sympathetic nervous system, the renin-angiotensin-aldosterone system, and the hypothalami-pituitary-adrenal axis and to contribute to risk of cardiovascular events.”
The researchers concluded that “more efforts are needed to understand the experiences of older adults with unstable housing and to estimate the scope of unstable housing among all individuals receiving dialysis.”
- Novick TK, Mader MJ, Johansen KL, et al. Unstable Housing and Mortality Among US Veterans Receiving Dialysis. JAMA Netw Open. 2023;6(11):e2344448. doi:10.1001/jamanetworkopen.2023.44448

