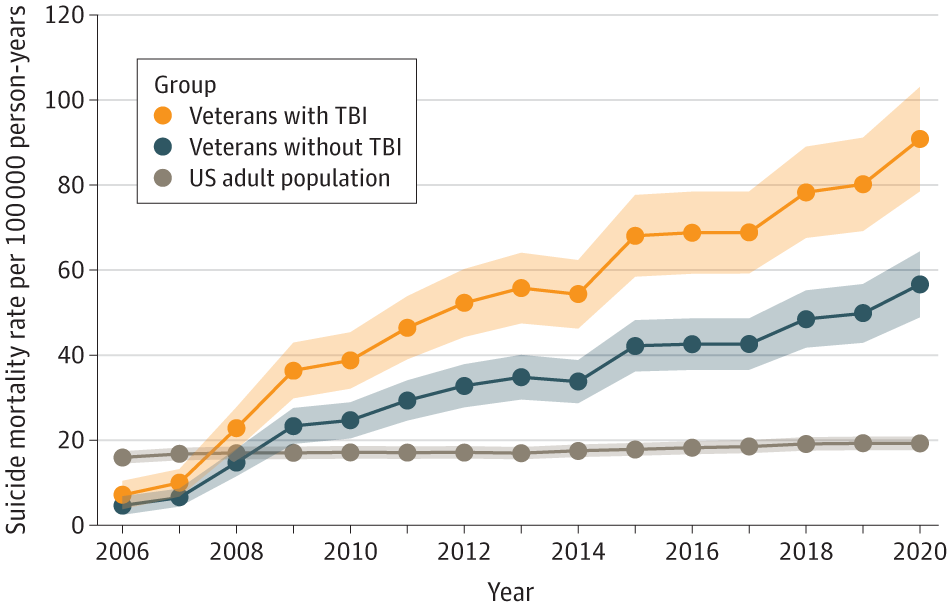
Click to Enlarge: Adjusted Suicide Mortality Rates per 100 000 Person-Years From 2006-2020 Average annual percentage change was 14.8% (95% CI, 10.5-19.2; P < .001) for veterans with traumatic brain injuries (TBIs), 14.4% (95% CI, 10.2-18.7; P < .001) for veterans without TBI, and 1.2% (95% CI, 0.9-1.4; P < .001) for the US adult population. Source: JAMA Network
BETHESDA, MD — As suicide deaths have reached shocking highs among American adults as a whole, the rates for U.S. veterans are even higher—57.3% greater than for nonveterans.
A new study suggested that veterans who have had traumatic brain injuries (TBIs) are particularly vulnerable, said co-author Ian J. Stewart, MD, PhD, a professor of medicine at Uniformed Services University in Bethesda, MD.
Stewart is an Air Force colonel, physician and researcher who has both treated combat injuries and dedicated a better part of his career to defining and evaluating long-term outcomes of soldiers who’ve suffered them. He is familiar with the effects of TBI, a common injury sustained both in the combat setting and in training environments, he said. In a 2021 study published in Brain and Behavior, Stewart and colleagues found traumatic brain injury was highly associated with subsequent development of PTSD, depression and anxiety.1
Because adverse mental health outcomes might lead to increased suicide risk, this finding prompted Stewart and his colleagues to explore both the rise in veterans’ suicides and the link between TBI and suicide in new research.
The recent study, which was published in JAMA Neurology, linked patients from the Military-Relevant Brain Injury Consortium Chronic Effects of Neurotrauma Consortium phenotype study—a large cohort of more than 2.5 million post-9/11-era veterans—to the National Death Index—a database of death and causes of death in the U.S. population. The researchers then stratified patients by TBI exposure and compared the suicide rates to the general population.2
“The key finding was that suicide rates are increasing through time in veterans compared to the general population,” Stewart said. A total of 8,262 suicide deaths among veterans and 562,411 among the U.S. adult population equated to crude rates of 42.13 and 18.42 per 100,000 person-years, respectively, he and his colleagues wrote. Suicide rates increased above 2006 levels beginning in 2008 through 2020 for veterans, and increased above 2006 levels beginning in 2012 through 2020 for the U.S. adult population.
Increased Risk With TBI
Furthermore, the study found that veterans with a history of TBI are at an increased risk compared to veterans without a history of TBI. From 2006-2020, suicide rates increased per year by 14.8% for veterans with TBI, 14.4% for veterans without TBI and 1.2% for the U.S. adult population.
From 2019-2020, suicide rates per 100,000 person-years increased from 80.16 to 90.81 for veterans with TBI and from 49.82 to 56.65 for veterans without TBI but did not change in the U.S. adult population, according to the report. Over the 15-year period from 2006 to 2020, veterans with TBIs had suicide rates three times higher than the U.S. adult population, the study showed.
The study does not answer why TBI is associated with suicide or why suicide rates would be rising after 9/11, but Stewart has some speculative answers. “I believe the answer is multifactorial,” he said. The first factor, he posited, is combat exposure. The data showed suicide rates for veterans start to increase above that of the general population in 2008. This corresponds to the “surge” in Iraq where large numbers of deployed servicemembers that saw combat, he noted. Second, he suggested that mental health—including disorders for which those injured in combat are at higher risk—must play a significant role in suicide.
Although the researchers only have data through 2020, Stewart said he suspects the increase in suicide risk has continued and will continue to rise over time.
“Veteran suicide has been a high-profile issue for several years, and there have been many efforts to stem this awful tide,” he said. “We need to develop alternate strategies to combat the issue. We need better tools for risk assessment and better therapeutics for mental health.”
“Until then,” Stewart said, “clinicians must have a high index of suspicion in the patients they care for that are post-9/11 veterans. Asking about suicidal ideation can be kind of like checking off a box and is often done in triage. Clinicians should build rapport and then ask the difficult questions themselves. It is uncomfortable, but the young men and women that volunteered to serve and in many cases sustained a TBI in the course of their service deserve nothing less.”
- Walker LE, Watrous J, Poltavskiy E, Howard JT, Janak JC, Pettey WBP, Zarzabal LA, Sim A, Gundlapalli A, Stewart IJ. Longitudinal mental health outcomes of combat-injured service members. Brain Behav. 2021 May;11(5):e02088. doi: 10.1002/brb3.2088. Epub 2021 Mar 4. PMID: 33662185; PMCID: PMC8119815.
- Howard JT, Stewart IJ, Amuan ME, Janak JC, Howard KJ, Pugh MJ. Trends in Suicide Rates Among Post-9/11 US Military Veterans With and Without Traumatic Brain Injury From 2006-2020. JAMA Neurol. 2023 Aug 28:e232893. doi: 10.1001/jamaneurol.2023.2893. Epub ahead of print. PMID: 37639278; PMCID: PMC10463169.

