Assistant Director Amanda Martinez, Employee Engagement Officer Kristen Luevanos and Voluntary Services Specialist Jill Schinski greet a veteran at a drive-thru baby shower line last year near Rocky Mountain Regional VAMC in Aurora, CO. VA photo.
WASHINGTON, DC — As of this month, mothers treated by the VA healthcare system pre- and post-partum have access to maternity care coordinators from the beginning of their pregnancy to 12 months after birth. That is a change from the previous end-date of 8 weeks post-partum.
No matter where the women give birth, the VA provides coordinators to help them navigate healthcare, find care after delivery, ensure access to follow-up screenings and help the expectant mothers understand costs and billing.
Part of the reason for the change was to comply with the White House Blueprint for Addressing the Maternal Health Crisis. Toward that goal, the VA also provides veterans with the full range of maternity care services throughout pregnancy, delivery, and postpartum – including primary care, exams, tests, ultrasounds, newborn care, lactation support, and more.
The fastest-growing cohort of veterans who use VA, about 600,000 receive healthcare from the VA. About half of those women are of child-bearing age, and pregnancies in women veterans using VA care have increased by more than 80% since 2014, from 6,950 pregnancies in 2014 to 12,524 in 2022.
“This expansion of care coordination is a critical step toward improving outcomes for Veteran mothers and their newborn children,” said Secretary of Veterans Affairs Denis McDonough. “Now, Veteran mothers will know that they have one-on-one support throughout every step of their pregnancy — from the day it begins to one year postpartum.”
“Evidence shows that new mothers often need support and care coordination long after 8 weeks post-partum, which is why VA is taking action to support Veteran mothers for much longer after they give birth,” said Under Secretary for Health Shereef Elnahal, MD. “We will also screen pregnant and postpartum veterans for social determinants of health, mental health risk factors, relationship health and safety, and more.”
VA maternity care coordinators also screen for social, physical, and mental health concerns and provide resources for childbirth education; and offer lactation consulting during pregnancy and after delivery.
Extended Follow-Up
“Extended follow-up care for postpartum Veterans is a great step forward, given that a significant proportion of poor maternal outcomes happen later in the postpartum period,” said Acting Chief Officer for VA Office of Women’s Health Sally Haskell, MD. “Extending postpartum care coordination up to one year allows VA maternity care coordinators the ability to double the amount of contact with their patients to help improve the physical and mental health of both parent and child.”
The VA previously reported that, while, the overall rates of pregnancy are lower in women veterans than in the general population (26.1 versus 34.4 per 1,000), their rates of an unplanned pregnancy is similar to women in the general population (37% compared to 35.2%).
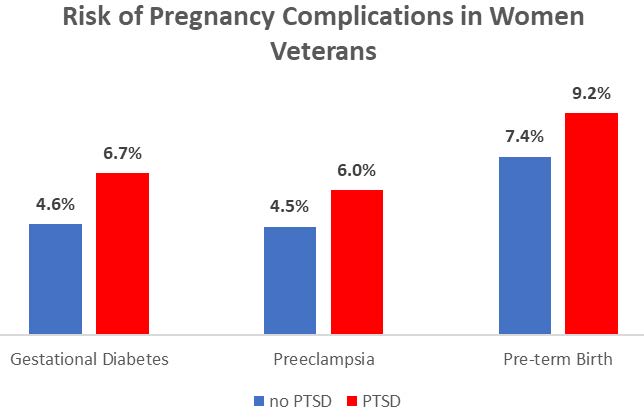
A complicating issue is that women veterans who receive maternity care through VA often have multiple medical conditions that can increase their risk of pregnancy complications. “Unique to veterans, experiencing a military deployment may increase the risk of pre-term birth,” according to a report from the VA’s Office of Health Equity. “It is suggested that one of the reasons for this increased risk of pre-term birth may be that being deployed also increases the risk of developing post-traumatic stress disorder (PTSD). Having PTSD can increase the risk of a spontaneous pre-term birth as well as preeclampsia and gestational diabetes.”
The Office of Health Equity pointed out that, in a cohort of more than 300 pregnant veterans across 15 VAMCs, nearly all (86%) used MCC services during their pregnancies. This cohort was racially and ethnically diverse (44% identifying as Black, Indigenous, People of Color (BIPOC) and 23% Hispanic) and 96% initiated breastfeeding/chestfeeding after their baby was born.
- Shaw, J.G., et al. Posttraumatic Stress Disorder and Risk of Spontaneous Preterm Birth. Obstetrics & Gynecology. December 2014 – Volume 124 – Issue 6 – p 1111-1119
- Shaw J.G., et al. Post-traumatic Stress Disorder and Antepartum Complications: a Novel Risk Factor for Gestational Diabetes and Preeclampsia. Paediatric & Perinatal Epidemiology. 2017 May;31(3):185-194.