Click to Enlarge: Abbreviation: AOR indicates adjusted odds ratio.
a. Among those reporting suicide ideation, suicide plans, or suicide attempts. Source: JAMA Network Open
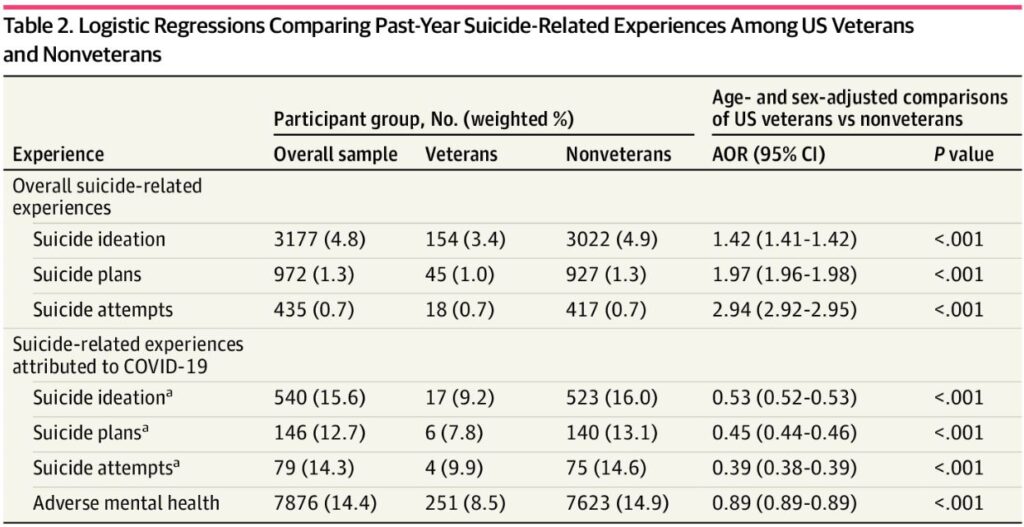
AURORA, CO — Veterans were more likely to report past-year suicidal ideation, plans and suicide attempts compared to nonveterans, but they were less likely to attribute their suicide-related experiences to the COVID-19 pandemic, according to a recent study.
The cross-sectional study published in JAMA Network Open investigated whether the COVID-19 pandemic impacted the mental health of military veterans differently than nonveterans. In particular, the researchers wanted to explore how the pandemic affected suicidal ideation, plans and attempts for veterans versus nonveterans, according to a study from the University of Colorado School of Medicine in Aurora and the Uniformed Services University in Bethesda, MD.1
Over the past two decades, the age- and sex-adjusted suicide rate for veterans have been higher compared to nonveterans, the VA reports. The COVID-19 pandemic prompted concerns about increased suicide risk, but the United States experienced declines in the suicide rate in 2019 and 2020 that were greater among veterans (9.7%) than nonveteran adults (5.5%), a university press release explained. However, a recent report found that “following this two-year decline, suicide rates increased in 2021, the last year for which data are available, among the general population.” Data on veterans are not yet published, according to the study.
In this study, the researchers analyzed data from the 2021 National Survey on Drug Use and Health (NSDUH), a survey of noninstitutionalized U.S. civilians 12 years and older. Data were collected from Jan. 14, 2021, to Dec. 20, 2021, and the researchers evaluated responses from 47,291 adults 18 years and older. The NSDUH excluded current active-duty military personnel, the study reported.
Veteran status was determined by a positive response to whether participants have ever been in the U.S. armed forces. Participants also were asked whether they had serious thoughts about suicide during the past 12 months (yes or no) and if they made a suicide plan or suicide attempt during the past 12 months (yes or no). For both of these questions, they were asked if this was because of the COVID-19 pandemic (yes or no). Participants also were asked how much, if at all, COVID-19 negatively affected their emotional or mental health since the beginning of the COVID-19 pandemic (not at all, a little, some, quite a bit or a lot).
The study found that, “while veterans were significantly more likely than nonveterans to report past-year suicidal ideation, plans and suicide attempts, veterans were significantly less likely than nonveterans to attribute their suicide-related experiences to the COVID-19 pandemic.” The researchers “attribute these findings to the ‘warrior mindset’ that comes with military experience,” according to the press release.
Veterans had 47% to 61% decreased odds of attributing their past-year suicidal experiences to the COVID-19 pandemic compared with nonveterans, the study reported.
Resilient to Psychosocial Effects
“From these findings, we may infer that many veterans are resilient to the psychosocial effects of tragedies, such as COVID-19, due to their military experiences, but it should not be lost that veterans still experience elevated rates of suicidal thoughts and behaviors compared with nonveterans,” Ian H. Stanley, PhD, assistant research professor in the Department of Emergency Medicine at the University of Colorado School of Medicine and the psychological health lead at the Center for Combat Medicine and Battlefield (COMBAT) Research at the University of Colorado Anschutz Medical Campus, said in the press release. “These findings underscore the need for a multilayered suicide prevention approach for this population.”
Stanley, also the military and veteran lead for the Firearm Injury Prevention Initiative at the University of Colorado School of Medicine, specializes in studying military communities and post-traumatic stress disorder. The study’s other two authors are military experts who have led trainings on resiliency and launched wellness initiatives for medical and military professionals, the press release reported.
The researchers said they hope to shift the “warrior mindset.”
Study co-author Kathleen M. Flarity, DNP, PhD, retired U.S. Air Force brigadier general and deputy director of the Center for COMBAT Research at the University of Colorado Anschutz Medical Campus, leads a resiliency training that has seen an uptick in enrollment since the COVID-19 pandemic. Flarity said she believes “military populations and other professions with high rates of compassion fatigue and burnout are still feeling the effects of the pandemic.”
“In so many cases, veterans don’t reach out and share their mental health struggles,” Flarity said. “We describe it as a ‘warrior mindset,’ which means doing whatever it takes to get through something traumatic. In one day alone, our servicemembers see what most of humanity does not see in a lifetime.”
In the resiliency trainings, Flarity “encourages participants to share their own experiences as a form of connection and healing.”
“Resiliency and seeking help go hand-in-hand; they’re signs of courage and strength,” Flarity said in the press release. “We are hoping the culture continues to transform in this next generation of servicemembers.”
Limitations of the study include “lack of data on the severity and chronicity of respondents’ suicidality, nuanced information on veteran status, and other potential contributors to respondents’ suicidal thoughts and behaviors,” according to the study.
- Stanley IH, Flarity KM, April MD. Suicide Ideation, Plans, and Attempts Attributed to the COVID-19 Pandemic Among US Veterans. JAMA Netw Open. 2023 Jun 1;6(6):e2320193. doi: 10.1001/jamanetworkopen.2023.20193. PMID: 37358856; PMCID: PMC10293906.

