Reasons for Disparity in Equal-Access VHA Remain Unclear
Click to Enlarge: Abbreviation: CT, computed tomography; LCS, lung cancer screening; LDCT, low-dose computed tomography.
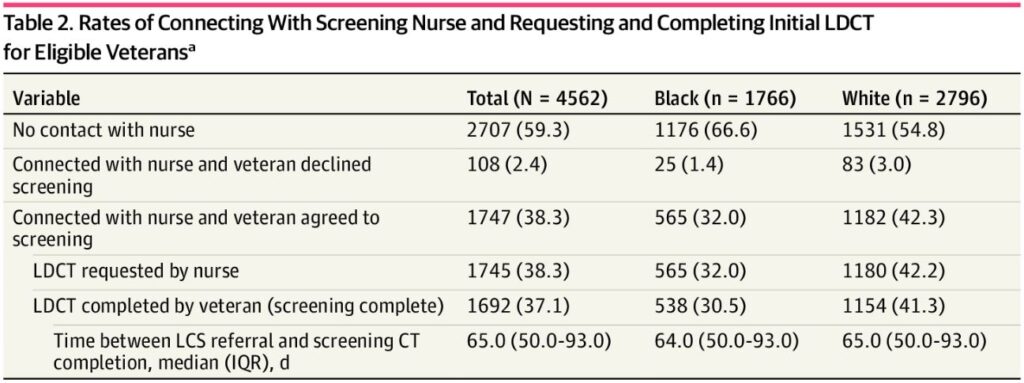
a. Data are presented as number (percentage) of patients, unless otherwise indicated. Source: JAMA Network Open
DURHAM, NC — Despite the VHA being an equal-access healthcare system, Black veterans in a recent study had considerably lower rates of lung cancer screening (LCS) than white ones. Yet, those differences aren’t fully explained by demographic and socioeconomic variables, the authors pointed out.
“This cross-sectional study found that, after referral for initial LCS via a centralized program, Black veterans had 34% lower odds of LCS screening completion compared with white veterans, a disparity that persisted even after accounting for numerous demographic and socioeconomic factors,” researchers from Duke University School of Medicine and the Durham, MC, VAMC explained. “A critical point in the screening process was when veterans must connect with the screening program after referral. These findings may be used to design, implement, and evaluate interventions to improve LCS rates among Black veterans.”
The cross-sectional study of 4,562 veterans eligible for and referred for lung cancer screening was conducted at the Durham VAMC, with results published in JAMA Network Open.1
Background information in the study advised that racial disparities in lung cancer screening often are related to barriers such as cost, insurance status, access to care and transportation. “Because these barriers are minimized within the Veterans Affairs system, there is a question of whether similar racial disparities exist within a Veterans Affairs health care system in North Carolina,” the authors wrote.
In response, the study team assessed veterans referred to LCS between July 1, 2013, and Aug. 31, 2021, at the Durham VA Healthcare System. All included veterans self-identified as white or Black and met the US Preventive Services Task Force eligibility criteria as of Jan. 1, 2021. Participants who died within 15 months of consultation or who were screened before consultation were excluded. The study defined screening completion was defined as undergoing computed tomography for LCS.
During the study period, 4,562 veterans, 94.2% male with a mean age of 65 were referred for LCS; of those, 38.7% were Black and 61.3% white. Of all veterans referred, 1,692 (37.1%) ultimately completed screening.
The study found that 59.3% “never connected with the LCS program after referral and an informational mailer or telephone call, indicating a critical point in the LCS process. Screening rates were substantially lower among Black compared with white veterans (538 [30.5%] vs. 1154 [41.3%]), with Black veterans having 0.66 times lower odds (95% CI, 0.54-0.80) of screening completion after adjusting for demographic and socioeconomic factors.”
That disparity persisted even after accounting for numerous demographic and socioeconomic factors, the authors pointed out. “Often-cited reasons for disparities in LCS rates include insurance status, rurality, environmental or occupational exposures outside of tobacco use, access to care and transportation, stigma, and challenges with patient-practitioner communication and shared decision-making,” according to background information in the report.
The study added that the Durham VAMC implemented a centralized LCS program in 2013 as part of a national program, and early data showed that 49.6% of eligible veterans across eight different sites received a screening CT scan, although results were not stratified by race. That finding compared with the estimated LCS rates of 5% to 17% nationally.
“Because several factors thought to be barriers to LCS, such as insurance status, screening cost, access to care and transportation, are minimized within the Veterans Affairs (VA) system, we sought to further examine racial disparities in LCS within the DVAHCS,” the researchers wrote.
Racial Disparities
They noted that their finding is consistent with other studies showing that those of Black race who meet guideline criteria for lung cancer screening are less likely to have that occur. In this study, the authors advised, “We report a similar racial disparity in LCS completion rates after accounting for various sociodemographic and clinical factors. This finding suggests that even though center characteristics, such as a centralized screening process or cost mitigation associated with a single-payer health system, may improve LCS rates overall, there are still racial disparities in LCS.”
The study suggested that the critical point for not completing screening within the VA’s centralized system is when individual veterans must connect with the LCS program to be scheduled for a low-dose CT scan. Nearly 60% of veterans never connect with the program after they receive a telephone call or informational mailer, the study added, with most agreeing to and completing LCS when they make contact.
“To try to understand which factors may help explain racial disparities in LCS, we assessed a wide array of variables,” the researchers recounted. “Age at LCS referral was the only variable for which the association with screening completion differed significantly by race. When looking at the odds of screening completion by race in the total cohort as well as the subgroup of Black veterans, veterans in older age categories had lower odds of screening completion compared with patients younger than 60 years. Potential reasons for this finding may include personal factors regarding attitudes around screening or cancer diagnosis, as well as practitioner factors around utility of screening and life expectancy.”
The study did not, however, capture social determinant of health including:
- educational level,
- health literacy,
- neighborhood-level data (eg, area deprivation index), and
- income.
“Other important variables likely include structural and systemic racism, implicit biases among clinicians, patient mistrust and skepticism, the racial and cultural environment of the health care setting, and differences in the quality of care among different racial groups,” the authors wrote. “These factors negatively affect Black veterans and their health-related behaviors and outcomes, but are difficult to measure or quantify, underscoring the need for further qualitative studies.”
They added that current smoking status at LCS referral and mental health or substance-use diagnosis were significantly associated with not screening in the total cohort multivariable analysis. “This finding is consistent with findings that current smokers are less likely to undergo guideline-concordant breast, prostate, or colorectal cancer screening compared with former smokers or never-smokers and that individuals with mental illness had lower cancer screening rates across a variety of cancer types, despite increased cancer mortality rates. It also underscores the need for targeted interventions, such as tailored counseling as described by Flores et al, for individuals with mental illness or substance use,” the study emphasized.
One notable finding was that higher pack-year smoking history was significantly associated with higher rates of screening completion, even after accounting for other covariates in the multivariable model. “For every 5 pack-years, a veteran had a 2% increase in the odds of screening completion”, the researchers revealed. “This finding is concerning given evidence that Black individuals develop lung cancer at lower pack-year histories. The updated USPSTF guidelines are an important step in engaging individuals with a 20- to 30-pack-year history, but further community engagement and implementation work are necessary.”
The study also pointed out that the costs of initial and annual low-dose CT scans for LCS are covered for veterans who are service connected by at least 50%. On the other hand, those with lower service connection percentages were required to pay a $50 co-payment for LCS during our study period. The result, according to the study, is that veterans with a service connection level of 50% to 100% were much more likely to complete screening than those with no service connection.
The VA recently announced that the cost of LCS would be covered for all patients regardless of percent service connection, “which will be an important step in decreasing loss to follow-up,” the researchers suggested.
- Navuluri N, Morrison S, Green CL, et al. Racial Disparities in Lung Cancer Screening Among Veterans, 2013 to 2021. JAMA Netw Open. 2023;6(6):e2318795. doi:10.1001/jamanetworkopen.2023.18795

