No Significant Effect on Acute Exacerbations Identified
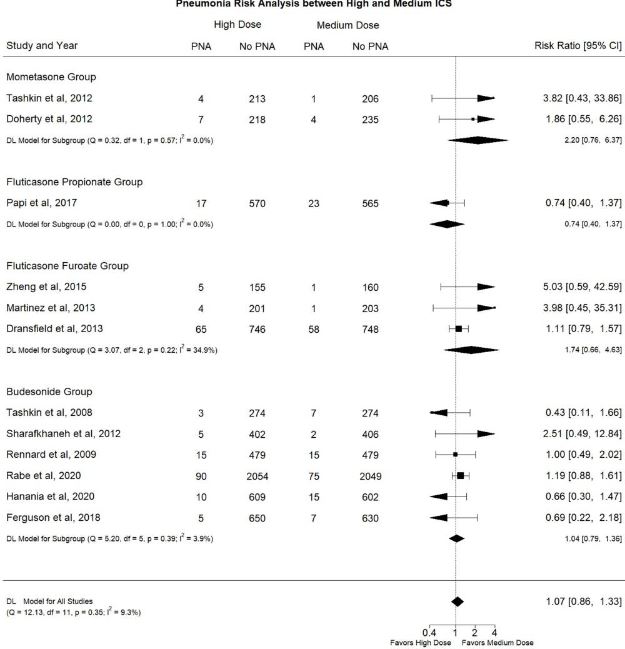
Click to Enlarge: Comparison of Pneumonia risk between patients with COPD using High Dose ICS versus Medium ICS as part of maintenance therapy. Source: International Journal of Chronic Obstructive Pulmonary Disease
IOWA CITY, IA — While inhaled corticosteroids (ICSs) combined with bronchodilators are known to improve outcomes in COPD, their use also can lead to certain adverse effects. That’s one reason a consensus on the optimal ICS dosing regimen has not been reached, according to a new study.
The VA Iowa City, IA, Healthcare System and colleagues performed a systematic review and meta-analysis to try to clarify the efficacy and safety of dosing levels—high vs. medium/low—of ICS with ancillary bronchodilators and in line with PRISMA guidelines.
Researchers systematically searched Medline and Embase until December 2021, including randomized, clinical trials (RCTs) that met predefined criteria. Included were trails with risk ratios (RRs) with 95% confidence intervals (CI).
“Any acute exacerbation of COPD (AECOPD) risk was chosen as the primary efficacy outcome, mortality rate as the primary safety outcome, moderate/severe AECOPD risk as the secondary efficacy outcome and pneumonia risk as the secondary safety outcome,” the authors explained, adding, “Subgroup analyses of individual ICS agents, of patients with baseline moderate/severe/very severe COPD and of patients with recent COPD exacerbation history were also performed. A random-effects model was used.”
Ultimately, 13 RCTs were included in the study, although no data on low doses were included in the analysis.
Results indicated that high dose ICS was not associated with a statistically significant difference in any AECOPD risk (RR: 0.98, 95% CI: 0.91-1.05, I2: 41.3%), mortality rate (RR: 0.99, 95% CI: 0.75-1.32, I2: 0.0%), moderate/severe AECOPD risk (RR: 1.01, 95% CI: 0.96-1.06, I2: 0.0%) or pneumonia risk (RR: 1.07, 95% CI: 0.86 -1.33, I2: 9.3%) compared to medium dose ICS. The authors pointed out that the same trend was identified with the several subgroup analyses.
“Our study collected RCTs investigating the optimal dosing level of ICS prescribed alongside ancillary bronchodilators to patients with COPD,” the researchers concluded. “We identified that the high ICS doses neither reduces AECOPD risk and mortality rates nor increases pneumonia risk relative to the medium dose.”
Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines have consistently recommended a stepwise approach to pharmacologic management of COPD in its stable state, using different inhaled medication classes, according to background information in the article.
Add-On Therapy
The use of an inhaled corticosteroid (ICS) is not the initial recommendation but is included as a second or third therapy, it added.
“The use of ICS is dictated by an individualized risks and benefits calculation. On one hand, they are effective in decreasing acute exacerbations of COPD (AECOPDs),” the authors advised. “AECOPDs are considered the most serious complication and a prevalent cause of mortality for patients with COPD, alongside cardiovascular causes and malignancies. On the other hand, ICSs have also been associated in a dose-dependent manner with potentially significant side effects, most importantly pneumonia but also others such as bone fractures and cataract.”
The authors noted that any effect on cardiovascular mortality has not yet been definitively established, although some evidence of all-cause mortality benefit associated with their use has recently become available.
Still, they pointed out that a consensus on the optimal ICS dosing regimen has not been reached.
“Our results provide a possibly significant contribution to the decision-making process of clinicians providing care to patients with COPD,” the researchers suggested. “According to the most recent GOLD guidelines, one of the main treatment goals for these patients is to tailor their inhaler maintenance regimen to prevent AECOPD, as per their multilevel detrimental effects. Combined ICS and bronchodilator therapy has been associated with improvement in lung function and health status, as well as reduction in exacerbations.”
The study also emphasized that ICS combinations increasingly are associated with all-cause mortality benefit. “Two recent large RCTs (IMPACT and ETHOS) showed reduction in all-cause mortality when ICS is added to dual bronchodilator therapy relative to dual bronchodilation therapy alone,” the researchers wrote. “The same conclusion was reached by a recently published meta-analysis that investigated all-cause mortality as the primary outcome.”
The importance of their study, according to the authors, is the finding that high ICS doses combined with bronchodilator therapy neither reduces AECOPD and mortality rates nor increases pneumonia risk relative to the medium dose. They called for further research to investigate whether low ICS doses can provide similar benefits with fewer adverse events than medium or high ICS doses to patients with COPD.
- Archontakis Barakakis P, Tran T, You JY, Hernandez Romero GJ, Gidwani V, Martinez FJ, Fortis S. High versus Medium Dose of Inhaled Corticosteroid in Chronic Obstructive Lung Disease: A Systematic Review and Meta-Analysis. Int J Chron Obstruct Pulmon Dis. 2023 Apr 6;18:469-482. doi: 10.2147/COPD.S401736. PMID: 37056683; PMCID: PMC10086393.

