Veterans Study Suggested GLP1RA Might Be Better
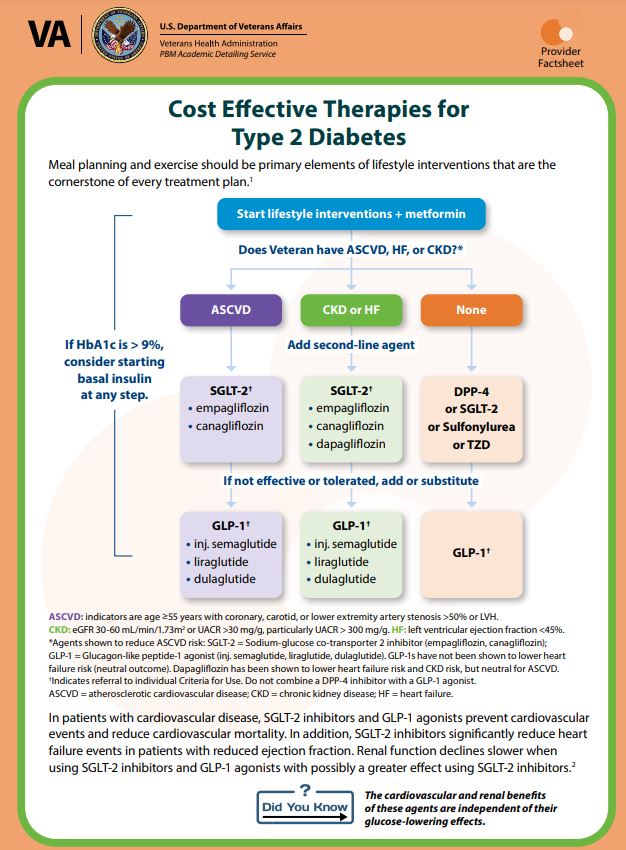
NASHVILLE, TN — In 2020, in its annual revision of the Standards of Medical Care in Diabetes, the American Diabetes Association (ADA) made some significant changes in recommendations. The association recommended that two drug classes be used to treat patients with Type 2 diabetes (T2D) and comorbidities: sodium-glucose co-transporter 2 inhibitors and. glucagon-like peptide-1 receptor agonists.
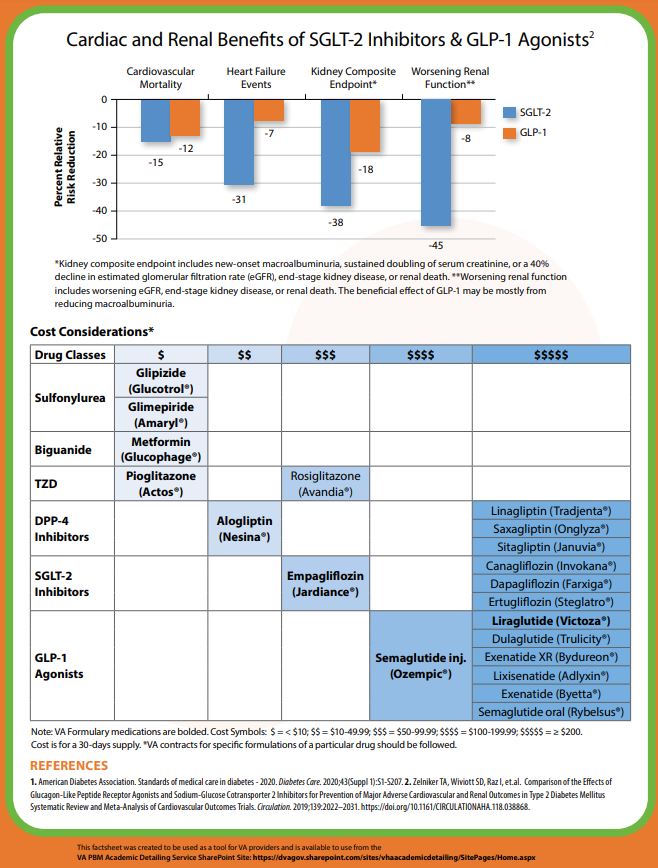
According to an article in The Lancet—Diabetes and Endocrinology, both treatments demonstrated “cardiovascular protection in dedicated outcome studies in patients with type 2 diabetes at high cardiovascular risk.”
Specifically, the ADA said the inhibitors “should be considered for patients when atherosclerotic cardiovascular disease (ASCVD), heart failure, or chronic kidney disease predominates independent of [glycated hemoglobin] A1C.”
A large new study recently looked at the effectiveness of glucagon-like peptide-1 receptor agonists (GLP1RA) and sodium-glucose cotransporter-2 inhibitors (SGLT2i) in preventing major adverse cardiac events (MACE) in a different cohort: U.S. veterans with T2D but without preexisting cardiovascular disease. The results are potentially practice-changing at the VA and elsewhere.
Researchers from the VA Tennessee Valley Healthcare System, the Vanderbilt University Medical Center and colleagues sought to test the hypothesis that MACE incidence was lower with the addition of GLP1RA or SGLT2i compared with dipeptidyl peptidase-4 inhibitors (DPP4i) for primary cardiovascular prevention.
Lead author Lee Richardson, MD, was quoted in a Vanderbilt press release as saying that two areas of uncertainty were addressed. He pointed out that many newer diabetes medications were tested versus a placebo, making it difficult to know whether one type offers an advantage over another. In addition, the clinical trials showing the cardiovascular benefits of the drugs were conducted in people who already had heart disease.
The retrospective cohort study included U.S. veterans from 2001 to 2019. Participants were adults receiving care from the Veterans Health Administration, with data linkage to Medicare, Medicaid and the National Death Index. Results were published in Annals of Internal Medicine.2
The patients, who were a median of 67 years old and had a median diabetes duration of 8.5 years, added GLP1RA, SGLT2i, or DPP4i onto metformin, sulfonylurea or insulin treatment alone or in combination. The cohort included 28,759 GLP1RA vs. 28,628 DPP4i weighted pairs and 21,200 SGLT2i vs. 21, 170 DPP4i weighted pairs. Episodes were stratified by a history of cardiovascular disease.
Defined as study outcomes were MACE (acute myocardial infarction, stroke or cardiovascular death) and heart failure (HF) hospitalization.
Lower MACE
Results indicate that glucagon-like peptide-1 receptor agonists were associated with lower MACE and HF vs. DPP4i (adjusted hazard ratio [aHR], 0.82 [95% CI, 0.72 to 0.94]), yielding an adjusted risk difference (aRD) of 3.2 events (CI, 1.1 to 5.0) per 1,000 person-years.
Sodium–glucose cotransporter-2 inhibitors were not associated with MACE and HF (aHR, 0.91 [CI, 0.78 to 1.08]; aRD, 1.28 [−1.12 to 3.32]) compared with DPP4i”, the researchers advised.
Essentially, the large observational study of U.S. veterans without preexisting heart disease found that glucagon-like peptide-1 receptor agonists seem to work best in preventing outcomes such as nonfatal stroke, nonfatal myocardial infarction and cardiovascular death. Sodium-glucose co-transporter 2 inhibitors were not found to be as effective.
One limitation of the study, according to the authors, is that the use of DPP4i, GLP1RA and SGLT2i as first-line therapies was not examined.
“The addition of GLP1RA was associated with primary reductions of MACE and HF hospitalization compared with DPP4i use; SGLT2i addition was not associated with primary MACE prevention,” the study concluded.
“We believe this study is an important contribution to patient care and adds to what we as clinicians know about treating diabetes and heart disease prevention,” added senior author Christianne Roumie, MD, MPH, a VA physician who also is a professor of Medicine in the Division of General Internal Medicine and Public Health at Vanderbilt.
- Scheen AJ. SGLT2 inhibitor or GLP-1 receptor agonist in type 2 diabetes? Lancet Diabetes Endocrinol. 2019 Nov;7(11):818-820. doi: 10.1016/S2213-8587(19)30310-9. Epub 2019 Sep 17. PMID: 31540866.
- Richardson TL Jr, Halvorson AE, Hackstadt AJ, Hung AM, et. al. Primary Occurrence of Cardiovascular Events After Adding Sodium-Glucose Cotransporter-2 Inhibitors or Glucagon-like Peptide-1 Receptor Agonists Compared With Dipeptidyl Peptidase-4 Inhibitors: A Cohort Study in Veterans With Diabetes. Ann Intern Med. 2023 May 9. doi: 10.7326/M22-2751. Epub ahead of print. PMID: 37155984.