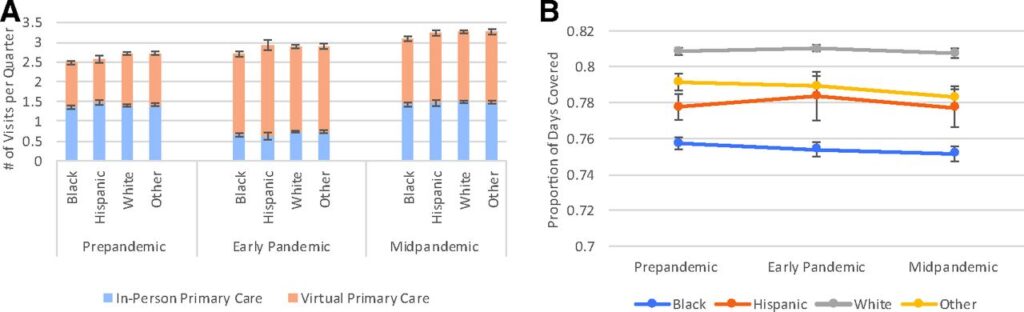
Click to Enlarge: Mean adjusted primary care visits (A) and medication adherence (B) in high-risk patients by race/ethnicity. In A, blue/orange bars show mean number of primary care visits per patient per quarter estimated from regression models. In B, adherence was measured by proportion of days covered, ranging from 0 to 1.0, per patient per quarter and estimated from regression models. Mean visits and adherence per quarter were estimated from linear regression models adjusting for age-group and pandemic phase and their interaction terms, quarter, patients’ sociodemographic characteristics, Elixhauser comorbidity, comorbid depression, distance to primary care site, rurality, clinic factors, and community rate of COVID infections. Source: Journal of The American Board of Family Medicine
PALO ALTO, CA — During the COVID-19 pandemic, high-risk diabetes patients who were treated in the VA Healthcare System adhered to their diabetes medication regimens and maintained high primary care use, even though virtual care replaced in-person care, according to a recent study.
The longitudinal study published in the Journal of the American Board of Family Medicine examined how diabetes medication adherence, related hospitalizations and primary care use changed in high-risk veterans before and after the COVID-19 pandemic, which potentially disrupted the care of chronic conditions.1
Most patients in the VAHS have chronic conditions (64%), and managing these conditions requires regular care, such as taking medications, and monitoring clinical measures. Because the COVID-19 pandemic led to pauses in many in-person services, the health of these patients was at risk for being impacted by disruptions to their care. Effective March 15, 2020, the VA issued a national directive to convert most in-person services to virtual (telephone or video), representing an abrupt change in care delivery.
The researchers followed a cohort of 188,569 high-risk diabetes patients in the VAHS over a three-year period, from Oct. 1, 2018, to Sept. 30, 2021. They studied patients who were identified as high-risk for hospitalization and death using a VA validated algorithm used to predict hospitalization and death. They also focused on patients with diabetes who had a history of using primary care in the VA system.
The patients were 95% male, 65% white and had a mean age of 68 years old. Only half were married, and most had a service-connected disability and lived in urban areas.
For this evaluation, the researchers used VA medical records and administrative data. They measured primary-care visits by modality, medication adherence and VA acute hospitalizations and emergency department visits. They also estimated differences among patients by race/ethnicity, age and rural/urban location.
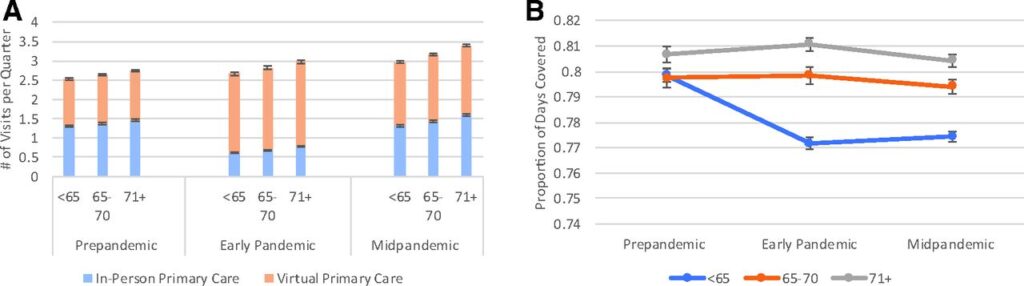
Click to Enlarge: Mean adjusted primary care visits (A) and medication adherence (B) in high-risk patients by age group. In A, blue/orange bars show mean number of primary care visits per patient per quarter estimated from regression models. In B, adherence was measured by proportion of days covered, ranging from 0 to 1.0, per patient per quarter and estimated from regression models. Mean visits and adherence per quarter were estimated from linear regression models adjusting for age-group and pandemic phase and their interaction terms, quarter, patients’ sociodemographic characteristics, Elixhauser comorbidity, comorbid depression, distance to primary care site, rurality, clinic factors, and community rate of COVID infections. Source: Journal of The American Board of Family Medicine
“We looked at veterans at high risk for hospitalization and death and found that they had high medication adherence for diabetes medications and similar levels of primary care utilization during the early and mid-pandemic periods although virtual care substituted for in-person primary care during the early pandemic period,” Jean Yoon, PhD, MHS, a health services researcher at the Palo Alto, CA, VA Healthcare System, told U.S. Medicine. “Patients had lower rates of hospitalizations during the early pandemic period.”
“We found that Black patients had the lowest adherence, and it decreased during the pandemic, unlike other racial/ethnic groups that did not have these changes,” Yoon said. “We also found that patients less than 65 years of age also had lower adherence during the pandemic. We were not able to determine the reasons why these patients had lower adherence compared to other patients.”
The study found that, per quarter, pre-pandemic patients had an average of 1.5 in-person primary care visits and 1.3 virtual visits, 0.10 hospitalizations and 0.22 emergency department visits, with mean adherence of 0.82. The early pandemic was associated with fewer in-person primary care visits, more virtual visits, fewer hospitalizations and emergency department visits per patient, and there was no change in adherence to diabetes medications. There were no mid-pandemic versus pre-pandemic differences in hospitalizations or adherence to diabetes medications. Also, Black and non-elderly patients had lower adherence to diabetes medications during the pandemic, according to the study.
The findings suggest that Black and non-elderly patients might require additional intervention to address lower adherence to diabetes medications.
Virtual Primary Care
“It appeared that many high-risk patients used virtual primary care, since there was a large increase in virtual care at the same time that in-person care decreased, even among older patients,” Yoon wrote in an email. “We did not find increases in hospitalizations for diabetes complications after the pandemic began, so there did not appear to be immediate, harmful effects using virtual care or disrupted care for patients. VA PACT teams and the tools they use to care for patients may have mitigated any potential harms to their care from the pandemic. However, we need to better understand why Black and non-elderly patients had lower adherence rates.”
The results suggested that primary-care clinics were largely successful in maintaining delivery of care to diabetic patients during the pandemic, according to the study.
“There were concerns that pandemic-related shutdowns of in-person care would be disruptive for sicker patients, but our results suggest there have been no early signs that primary care was disrupted for many high-risk patients,” Yoon wrote in an email.
Yoon said she believes that it’s important for healthcare professionals caring for high-risk diabetes patients to understand whether there might be long-term effects of the pandemic on patients’ health.
“While we didn’t see any evidence in the short-term, providers caring for high-risk patients should continue to assess their patients’ clinical measures and health care needs as we recover from the pandemic,” she advised.
Lessons learned from the VA experience with virtual care rollout can help mitigate negative impacts of increased virtual care use for all patients with chronic health conditions. The VA’s salaried staffing model, established primary-care practices around panel management, prior experience with virtual modalities, low cost-sharing for care and providing medications through the mail may have mitigated adverse impacts on patients’ access to primary care and crucial medications during the shutdown of in-person services. Though some of these features are unique to the VA system, other healthcare organizations can use some of the features, such as team-based models of care, mail delivery for medication refills and reduced cost-sharing for the sickest patients, to improve care during regular times and disasters, according to the study.
A key area of concern was that Black patients had lower rates of diabetes medication fills than white patients, and the difference widened during the pandemic. That could indicate that strategies or systems that mitigated gaps in medication adherence were not made as accessible, or were used at lower rates, by minority veterans, according to the authors. Proactive and effective interventions, such as clinical pharmacist monitoring, automated refills and combination pills to reduce pill burden, could be prioritized for Black patients and clinics that serve a higher percentage of minority patients, the study recommended.
- Yoon J, Chen C, Chao S, Wong E, Rosland AM. Adherence to Diabetes Medications and Health Care Use During the COVID-19 Pandemic Among High-Risk Patients. J Am Board Fam Med. 2023 Apr 3;36(2):289-302. doi: 10.3122/jabfm.2022.220319R1. Epub 2023 Mar 3. PMID: 36868867.

