Death Rates Were Compared Between Veterans, General Population
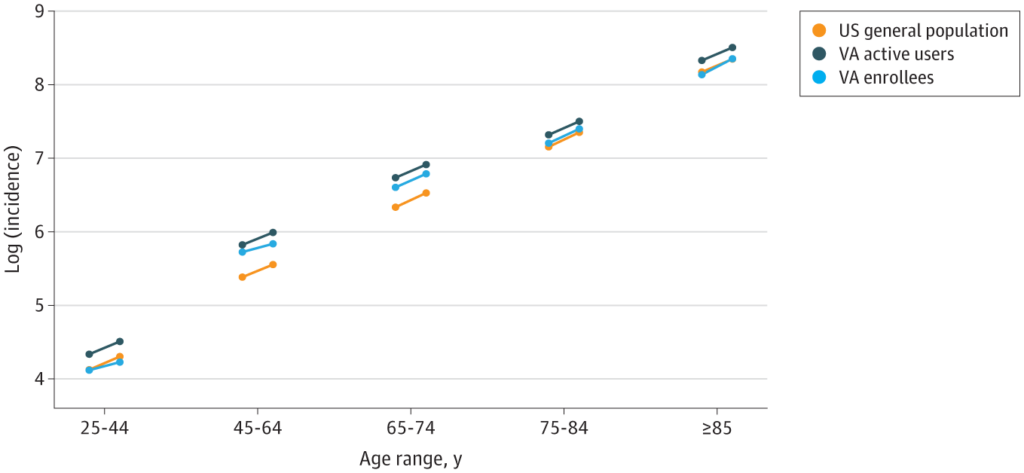
Click to Enlarge: Circles on the left sides of the lines are expected mortality rates, and circles on the right sides of the lines are observed mortality rates. The slope of the line indicates the relative increase during the pandemic (the risk ratio). Mortality rates are standardized based on the sex, race and ethnicity, region, and distribution of the 65- to 79-year VA enrollee population. Parallel slopes of the lines indicate a similar relative increase (risk ratio). Source: JAMA Network Open
NEW HAVEN, CT — Early in the COVID-19 pandemic, some concerns were raised about whether the VHA was experiencing a greater increase in mortality rates relative to the general population.
A new cohort study has put that hypothesis to rest. An article in JAMA Network Open reported that changes in death rates between the VA population and the general U.S. population were comparable after accounting for demographic differences between the populations. The VHA treats a higher percentage of older men.1
“The changes varied by race and ethnicity in both populations; these disparities changed over time,” wrote the study team, which was led by researchers from the Yale School of Public Health in New Haven, CT, and the VA Connecticut Healthcare System in West Haven, CT.
Public health officials were alarmed during the first year of the COVID-19 pandemic, by the substantial increase in the rate of death in the United States. “It is unclear whether those who had access to comprehensive medical care through the Department of Veterans Affairs (VA) health care system had different death rates compared with the overall US population,” the authors explained.
In response, they sought to quantify and compare the increase in death rates during the first year of the COVID-19 pandemic between patients receiving comprehensive medical care through the VHA and those in the general U.S. population.
“There are reasons to think that the outcomes for the VA active user population would have been more associated with the COVID-19 pandemic compared with the general U.S. population,” the study team suggested. “The VA population is heavily skewed toward men, has a high prevalence of comorbid conditions, and is enriched for those seeking medical care. All these factors can increase the risk of severe outcomes from COVID-19.” Yet, it added, “The baseline death rate was higher in the VA populations, but the relative increase during the pandemic was not notably different.”
Included in the study were 10.9 million enrollees in the VA, including 6.8 million active users of VA health care, defined as those with a visit in the last two years. The veterans cohort was compared to the general population of the United States. The focus was on deaths occurring from Jan.1, 2014, to Dec. 31, 2020.
The researchers analyzed changes in rates of death from any cause during the COVID-19 pandemic in 2020 compared with prior years. Age, sex, race and ethnicity, and region, based on individual-level data, were used to stratify changes in all-cause death rates.
One big difference was demographic characteristics, according to the report. The VA populations were predominantly male (>85% in the VA healthcare system vs. 49% in the general U.S. population), older (mean [SD], 61.0 [18.2] years in the VA healthcare system vs. 39.0 [23.1] years in the U.S. population) and had a larger proportion of patients who were white (73% in the VA healthcare system vs. 61% in the U.S. population) or Black (17% in the VA healthcare system vs. 13% in the U.S. population).
“Increases in death rates were apparent across all of the adult age groups (≥25 years) in both the VA populations and the general U.S. population,” the authors wrote. “Across all of 2020, the relative increase in death rates compared with expected values was similar for VA enrollees (risk ratio [RR], 1.20 [95% CI, 1.14-1.29]), VA active users (RR, 1.19 [95% CI, 1.14-1.26]), and the general U.S. population (RR, 1.20 [95% CI, 1.17-1.22]). Because the pre-pandemic standardized mortality rates were higher in the VA populations prior to the pandemic, the absolute rates of excess mortality were higher in the VA populations.”
The study concluded that active users of the VA health system had similar relative increases in mortality compared with the general U.S. population during the first 10 months of the COVID-19 pandemic.
Higher Among Older Adults
Background information in the report pointed out that, during the first year of the COVID-19 pandemic, the rate of death in the United States increased substantially. “This increase, particularly among older adults, was largely a consequence of infection with SARS-CoV-2,” the researchers explained. “However, the association of the pandemic with death rates varied substantially across subpopulations. Rates of death related to COVID-19 were higher among Black and Hispanic populations compared with white populations, among men compared with women, and among older adults compared with younger individuals.”
They added, “These disparities were associated with many factors, including social determinants of health (e.g., employment type and household composition), differing comorbidities, systemic differences in access to health care, and biological differences in immune responses by age and sex.”
Interestingly, according to the article, some previous reports suggested that death rates among those who typically received care in the VA health system were less affected than death rates among the general U.S. population during the COVID-19 pandemic, despite higher rates of comorbidities in the veteran population.
“However, veterans enrolled in VA healthcare also differ from the general U.S. population in age, sex, racial and ethnic composition, and geographic distribution, and each of these factors has been associated with mortality rates in general and death rates due to COVID-19 specifically,” the study team advised. “Using detailed data on individual deaths, it is now possible to make appropriate comparisons by accounting for the differing demographic characteristics of veterans receiving care from the VA health system vs. individuals in the general U.S. population.”
The researchers said their analysis “demonstrated that the COVID-19 pandemic effectively acted as a multiplier on the baseline death rates” and suggested that future studies might focus on estimating excess deaths with individual-level analysis, evaluating variations with comorbid conditions.
“Although this type of analysis would be challenging to do in the general U.S. population due to a lack of electronic health records, the VA health system is well equipped to do so,” they added.
Researchers from the Palo Alto, CA, and the White River Junction, VT, VAMCs also participated in the study.
- Weinberger DM, Rose L, Rentsch C, et al. Excess Mortality Among Patients in the Veterans Affairs Health System Compared With the Overall US Population During the First Year of the COVID-19 Pandemic. JAMA Netw Open. 2023;6(5):e2312140. doi:10.1001/jamanetworkopen.2023.12140


