Immune checkpoint inhibitors have played a major role in the increased survival of patients with NSCLC. Now, a new study looking at veterans has raised the possibility that common painkillers, nonsteroidal anti-inflammatory drugs (NSAIDs), could play a role in further lengthening survival rates in lung cancer patients being treated with ICIs.
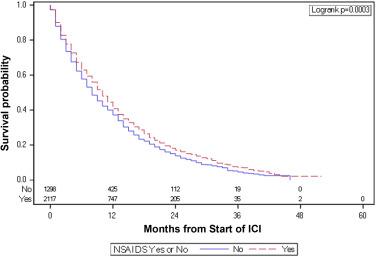
Click to Enlarge: Kaplan-Meier curves for overall survival, comparing all patients who received NSAIDs and those who did not receive NSAIDs. Hazard ratio = 0.87; 95% CI 0.81 – 0.94; p < 0.001. Source: Clinical Lung Cancer
ATLANTA — For veterans, the rate of lung cancer is even higher than for the general population, according to the VA. Nearly 8,000 veterans are diagnosed and treated in the VA for lung cancer each year. An estimated 900,000 are at risk for lung cancer due to age, smoking and environmental exposures during and after military service. For veterans with lung cancer, the rate of survival also is lower than for the general population.
Although the advent of immune checkpoint inhibitors (ICIs) has led to substantial improvements in lung cancer survival over the past decade—particularly in patients with metastatic and locally advanced non-small cell lung cancer (NSCLC) —not all people respond to the drugs. And the majority of those who do eventually have disease progression, possibly due to development of tumor resistance to further immune blockade, said Nikhil T. Sebastian, MD, assistant professor of radiation oncology at Emory Winship Cancer Institute in Atlanta and first author of a new study suggesting the use of nonsteroidal anti-inflammatory drugs (NSAIDs) may prolong survival in NSCLC patients taking immune checkpoint inhibitors.1
“Our group is interested in identifying drugs that can easily be repurposed which are well tested, widely available and affordable drugs that could potentially enhance these immune checkpoint inhibitors,” he said.
In the joint study of the Atlanta VAMC and Emory University’s Winship Cancer Institute and Morningside Center for Innovative and Affordable Medicine, Sebastian and his colleagues used the VHA Corporate Data Warehouse to identify patients who were diagnosed with NSCLC between 2010 and 2018 and treated within the VA system. They stratified patients between those with concomitant NSAID use—defined as NSAID dispensation by a VA pharmacy within 90 days of any ICI infusion—and those without. Survival was measured from the start of ICI.
Overall Survival
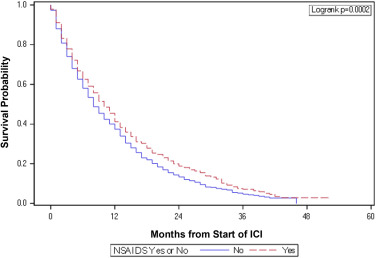
Click to Enlarge: Kaplan-Meier curves for overall survival, comparing propensity-score matched patients who did and did not receive NSAIDs. Hazard ratio = 0.85; 95% CI 0.78 – 0.92; p < 0.001. Source: Clinical Lung Cancer
The researchers then used various statistical analyses to compare the survival of the two groups, Sebastian said. “In total we identified 3634 veterans with non-small lung cell cancer and close to two-thirds of them were treated with NSAIDs. Those treated with NSAIDs had a higher number of medical comorbidities and in general were sicker patients,” he said. Yet, interestingly, they had overall survival—a mean of 10 months as opposed to eight—compared to those who didn’t receive NSAIDs. Results were published in the journal Clinical Lung Cancer.
When the researchers stratified NSAIDs by individual subtype, diclofenac was the only one that had a statistically significant association with overall survival, Sebastian said, noting that the study wasn’t designed to study individual NSAIDs. “We didn’t have enough patients per group, but it is an interesting correlation nonetheless,” he said.
The theoretical rationale for why NSAIDs in general work is that they block cyclooxygenase, said Sebastian. Preclinical studies suggest that cyclooxygenase-dependent pathways mediate tumor growth and evasion of immunity. “So blocking this enzyme with NSAIDs could theoretically enhance anti-tumor immunity,” he said.
The increased survival associated with diclofenac use in particular might be due to its unique effects on cellular lactate secretion, he said. “In theory, decreasing lactate in the tumor microenvironment can also enhance tumor immunity.”
“I think it is a promising finding in that we found a class of drug that is safe, affordable and widely available that may improve survival in this group of patients,” he said, while also noting that the study showed a correlation and “correlation is not a causation.”
“I think the only way to really properly determine if NSAIDs can improve survival in this group is to do a randomized controlled clinical trial,” Sebastian said. “It is hard to extrapolate from this kind of retrospective data the difference in survival because there are so many different confounding factors that may be affecting those numbers.”
Eventually, prescribing NSAIDs might be found to improve efficacy of ICI in patients with NSCLC. “But until we get a clinical trial, I don’t know that we can make a recommendation regarding NSAIDs one way or another,” said Sebastian, adding that he hopes such a trial could be started soon.
- Sebastian NT, Stokes WA, Behera M, Jiang R, Gutman DA, Huang Z, Burns A, Sukhatme V, Lowe MC, Ramalingam SS, Sukhatme VP, Moghanaki D. The Association of Improved Overall Survival with NSAIDs in Non-Small Cell Lung Cancer Patients Receiving Immune Checkpoint Inhibitors. Clin Lung Cancer. 2023 Jan 21:S1525-7304(23)00001-3. doi: 10.1016/j.cllc.2022.12.013. Epub ahead of print. PMID: 36804711.
