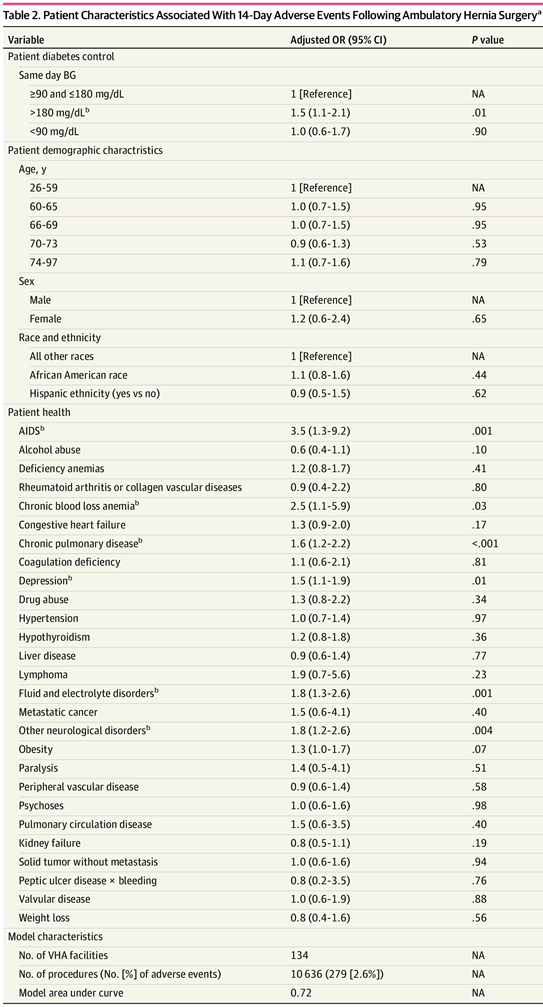
Click to Enlarge: Patient Characteristics Associated With 14-Day Adverse Events Following Ambulatory Hernia Surgery
Abbreviations: BG, blood glucose; OR, odds ratio; NA, not applicable; VHA, Veterans Health Administration.
SI conversion factor: To convert milligrams per deciliter of BG to millimoles per liter, multiply by 0.0555.
a. The analysis was performed using logistic regression models with facility fixed effects. Data are from all ambulatory hernia procedures performed in the VHA between October 1, 2015, and September 30, 2019, for patients with diabetes. Insignificant temporal risk-adjuster variables are not presented.
b. Statistically significant at P < .05.
Source: JAMA Network Open
BOSTON — An estimated 1 in 10 Americans and 1 in 4 veterans has diabetes, not only putting them at increased risk for problems such as heart and kidney disease, but also making them more prone to complications such as infection and bleeding following surgery.
For that reason, several academic societies recommend testing glycemic control preoperatively; however, there had been limited evidence that keeping within recommended blood glucose (BG) concentrations of 100 to 180 mg/dL is associated with improved outcomes in ambulatory surgery. Now, a new cohort study of veterans with diabetes undergoing ambulatory hernia surgery bolsters that evidence.
While hernia repair is a commonly performed procedure with a low rate of adverse events, the risk of complications including infection, bleeding and superficial wound dehiscence is higher for patients with Type 1 or Type 2 diabetes.
To determine whether poor same-day preoperative glycemic control was associated with higher odds of postoperative adverse events among VA patients undergoing the surgery, Boston VA Healthcare System-led researchers analyzed data from VHA Corporate Data Warehouse for patients undergoing hernia repair procedures between Oct.1, 2015, and Sept.30, 2019. The cohort consisted of 12,654 patients who underwent a total of 13,100 hernia repair procedures at 137 VHA facilities. Most procedures were performed in patients who were male (97%) and white (74.4%).1
The group defined poor diabetes control by two separate measures: same-day blood glucose concentration of lower than 90 mg/dL (hypoglycemic) and higher than 180 mg/dL (hyperglycemic). The primary outcome for the study published in JAMA Network Open was any surgical adverse event (wound-related complication, peritoneal abscess, bleeding, bacterial pneumonia, urinary tract infection and sepsis) based on relevant diagnosis codes from admission, emergency department or outpatient visit within 14 days of the procedure.
Of the 13,100 procedures, 576 (4.4%) were for patients with same-day preoperative hypoglycemia, 1,507 (11.5%) were for patients with same-day preoperative hyperglycemia, the group found. Preoperative blood glucose laboratory data were missing for 2,464 procedures (18.8%).
At least one 14-day adverse event occurred for 339 procedures (2.6%). Risk-adjusted odds of an adverse event were higher for patients with same-day preoperative hyperglycemia (adjusted odds’ ratio, 1.5 [95% CI, 1.1-2.1]). The study found no association between postoperative adverse events and same-day hypoglycemia.
The new study’s complication rate of 2.6% is lower than that of a Swedish registry study (4.7%)—a difference which may be explained by exclusion of emergent and inpatient hernia procedures, the authors wrote.
The study was limited by a disproportionately white and male VA population compared with the general public, and “potentially relevant clinical details were not included in risk adjustment (e.g., wound class, component separation, duration of surgery, or mesh size),” according to the authors.
“The findings of this cohort study suggest that an elevated preoperative glucose level was associated with an elevated risk of adverse events following ambulatory hernia surgery,” the researchers concluded. “Patient education on preoperative glucose management and team training to ensure glucose assessment on the day of surgery and potential intervention for hyperglycemia may present opportunities to decrease the number of postoperative adverse events.”
- Shanahan J, Vimalananda VG, Graham L, Schumann R, Mull HJ. Association Between Preoperative Diabetes Control and Postoperative Adverse Events Among Veterans Health Administration Patients With Diabetes Who Underwent Elective Ambulatory Hernia Surgery. JAMA Netw Open. 2023 Mar 1;6(3):e236318. doi: 10.1001/jamanetworkopen.2023.6318. PMID: 37000453; PMCID: PMC10066455.

