SAN FRANCISCO — The burden of cardiovascular disease among HIV patients has tripled over the past few decades, and cardiovascular mortality has steadily risen.
The findings of a new study further complicated the issue. It found that HIV patients with obstructive coronary artery disease have worse long-term survival after percutaneous coronary intervention (PCI) compared to patients who don’t have HIV.
The study published in the Journal of the American Heart Association sought to compare real-world treatment of coronary artery disease, as well as patient and procedural factors and outcomes after minimally invasive PCI between people living with HIV and uninfected controls.1
Even with antiretroviral therapy, HIV infection is associated with a higher risk of atherosclerosis, acute myocardial infarction, peripheral artery disease, ischemic stroke and sudden cardiac death. It’s critical to identify therapeutic strategies to improve cardiovascular outcomes in this high‐risk population, according to the study.
The researchers used data from the VA Clinical Assessment, Reporting, and Tracking (CART) Program, a mandatory national quality and safety program for procedures performed in cardiac catheterization laboratories throughout the entire VA Healthcare System. The data from Jan. 1, 2009, to Dec. 31, 2019, analyzed 184,310 patients with obstructive coronary artery disease on angiography.
Outcomes in people living with HIV undergoing PCI have not been widely studied, according to the authors.
“This study found that persons with HIV had worse long-term survival following percutaneous coronary intervention (PCI) despite having fewer traditional risk factors, similar types of procedures and well-controlled HIV disease,” Priscilla Y. Hsue, MD, study author and a professor at the University of California, San Francisco, School of Medicine, told U.S. Medicine.
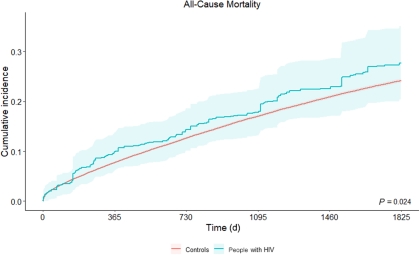
“Our study extends upon data in the field by looking at longer-term outcomes and was able to also evaluate the impact of HIV disease characteristics and procedural factors to show that persons with HIV had a greater than 20% higher mortality risk at five years,” Hsue wrote in an email.
Despite the study’s findings, Rushi Parikh, MD, lead author of the study and assistant clinical professor in the Division of Cardiology at the University of California, Los Angeles, told U.S. Medicine that it was “reassuring to see no evidence of health inequity between HIV+ and HIV-patients with respect to PCI procedural metrics, such as the type of stent used or antiplatelet medicines administered in the current era.”
“These types of care gaps have been previously shown in older datasets,” Parikh noted in an email.
Among patients with obstructive coronary artery disease, treatment strategy was similar between people living with HIV and controls. For percutaneous coronary intervention, 35.7% of people living with HIV versus 34.2% of controls received this treatment. For coronary artery bypass grafting, 13.6% of people living with HIV versus 15% of controls received this treatment. For medical therapy, 50.7% of people living with HIV versus 50.8% of controls received this treatment.
Well-Controlled HIV
People living with HIV undergoing PCI tended to have had well‐controlled HIV disease. Compared with controls, they were younger, more likely to be Black and had fewer traditional risk factors, more acute coronary syndrome, less extensive coronary artery disease and similar types of stents and P2Y12 therapy.
Despite well‐controlled HIV disease, a more favorable overall cardiovascular risk profile and similar percutaneous coronary intervention procedural metrics, HIV patients still have significantly worse long‐term survival following percutaneous coronary intervention than controls, the researchers noted. The study found that people living with HIV experienced worse survival as early as 6 months post‐PCI, which persisted over time and amounted to a 21% increased mortality risk by 5 years (hazard ratio, 1.21 [95% CI, 1.03-1.42; P=0.02]).
This study offered some recommendations to healthcare professionals treating coronary artery disease in people living with HIV.
“Clinicians caring for persons with HIV should be aware of heightened risk of CAD as well as worsened outcomes following intervention during cardiac catheterization,” Hsue explained. “Controlling all traditional risk factors is critical, including treatment of blood pressure, lipids, diabetes, weight and smoking to prevent disease. Furthermore, careful observation of symptoms and partnership with cardiology pre- and post-procedure as part of a team approach will help to reduce risk before clinical events and also improve outcomes after cardiac intervention.”
Additional studies are needed to determine underlying issues that cause persons with HIV to have worse long-term survival following percutaneous coronary intervention and identify causes of death. This will help improve outcomes in this high-risk population, Hsue wrote in an email.
“HIV physicians, cardiologists and researchers should be aware of this heightened risk for mortality following PCI procedures in HIV,” Hsue pointed out. “More studies are needed to determine factors underlying this increased risk, which may be due to chronic inflammation, immune activation and other issues, as a means to reduce risk and improve outcomes in persons with HIV.”
The lack of major differences in percutaneous coronary intervention procedural metrics between people living with HIV and the general population suggested that newer treatment strategies should be considered to improve survival in this high‐risk population, according to the study.
Among the limitations of the study, the VA CART Program only captured data on patients undergoing cardiac catheterization, and the data lacked granularity to discriminate the cause of death (cardiovascular versus non-cardiovascular). Also, women were substantially underrepresented in this study, which make the findings less generalizable to non-veteran populations.
- Parikh RV, Hebbe A, Barón AE, Grunwald GK, Clinical Characteristics and Outcomes Among People Living With HIV Undergoing Percutaneous Coronary Intervention: Insights From the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program. J Am Heart Assoc. 2023 Feb 21;12(4):e028082. doi: 10.1161/JAHA.122.028082. Epub 2023 Feb 15. PMID: 36789851.