Includes Increased Risk for Accidents, Violence
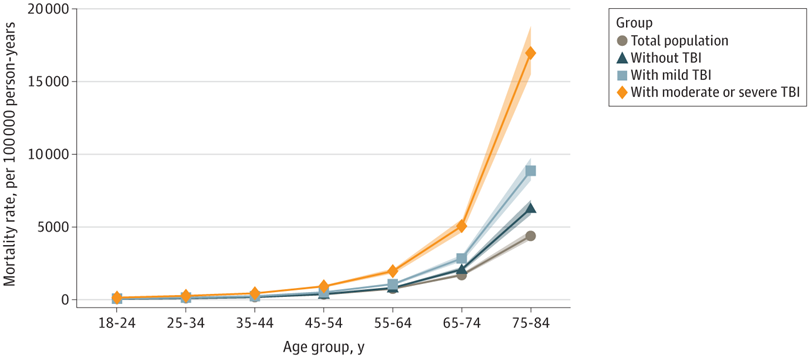
Click To Enlarge: Shaded areas indicate 95% CIs. Source: Howard, JT; Stewart, IJJ.; Amuan M; Janak JC; Pugh MJ. Association of Traumatic Brain Injury With Mortality Among Military Veterans Serving After September 11, 2001. JAMA Network Open. Published February 11, 2022. DOI: 10.1001/jamanetworkopen.2021.48150.
SAN ANTONIO — In the 20th century, military servicemembers were found to be healthier than the average individual, with lower mortality rates than their U.S. civilian counterparts. But new evidence shows that, since 9/11, U.S. veterans, particularly those who experienced traumatic brain injury (TBI), are dying at higher rates than the general population.
Combat-related traumatic brain injury is considered a signature wound of the Global War on Terror, as a result of the increased use of improvised explosive devices. During the same period, medical advances and improvements in body armor have allowed servicemembers to survive severe injuries that once would have been fatal, which has led to a surge in disabilities among veterans. The number of post-9/11 military veterans with service-connected disabilities is estimated to be 1.8 million, more than double the number from the first Gulf War and triple the number from previous wars.1
For the past decade, a team of researchers including Jeffrey Howard, PhD, associate professor of public health at the University of Texas-San Antonio, have been studying the long-term health consequences in servicemembers exposed to combat trauma. Their prior research has shown the cohort of soldiers who served after 9/11 and were exposed to trauma has an increased risk of a variety of chronic health issues.2
“Seeing that pattern emerge led us to ask whether that’s also translating into premature or excess mortality,” Howard said. In a new study, published in JAMA Network Open, the researchers examined 17 years of administrative and mortality data for more than 2.5 million veterans who served after 9/11, analyzing mortality rates, as well as the number and cause of excess deaths, among veterans both with and without TBI.3
The study included veterans who required multiple years of treatment or care in the MHS and/or the VHA. Data from the Veterans Affairs/Department of Defense Repository, health records data from the Military Health Service Management Analysis and Reporting Tool, the VHA Veterans Informatics and Computing Infrastructure and the National Death Index was compared with information from the national Centers for Disease Control and Prevention’s WONDER database for the total U.S. population.
Among post-9/11 veterans, the team found more than 3,800 excess deaths, or deaths over and above what would be expected during the study period. Most of those deaths were attributable to accidents and suicide, which were also the top two causes of death for veterans. Veterans with moderate to severe TBI accounted for more than one-third of total excess deaths—11 times higher than would otherwise be expected. Excess deaths were also concentrated in younger veterans between the ages of 18 and 44.
The other leading causes of death for veterans were cancer, cardiovascular disease and homicide. The mortality rates for each of these causes were higher among veterans with moderate to severe TBI compared with veterans without TBI. Howard says the team was surprised by some of the findings.
“Based on our prior research, we hypothesized that individuals who were exposed to more severe TBI would have elevated mortality for cardiovascular disease, and we did find that. But it wasn’t the main driver of excess mortality—it was accidents,” he said. “To have accidents as a leading cause of death among a younger cohort isn’t surprising, but the extent of the excess deaths compared to similar aged groups within the total U.S. population was surprising.”
Similarly, previous research has indicated that veterans are at higher risk for suicide than civilians. Yet the mortality rate, particularly among those veterans with moderate to severe TBI (81.5 per 100,000 person-years), was strikingly higher than that of the general population (15.9 per 100,000 person-years). But perhaps the most startling finding was that veterans with TBI had a more than threefold risk of being murdered compared to average Americans.
“We did not expect to see that,” Howard pointed out. “The study didn’t provide enough detail to really understand the circumstances that led to those outcomes, but just the fact that we’re seeing such high homicide rates for this cohort was shocking and, quite frankly, disturbing.”
The findings highlight the importance of investigating the factors that are driving veterans’ increased mortality risk, especially veterans who are exposed to traumatic combat injuries. Howard noted that there’s still a lot that experts don’t know about how TBI affects veterans.
“Much of the research on TBI has focused on things like treatments and medical care, but this is a multidimensional problem,” he said. “There’s a need to understand a much wider array of issues, including social conditions.”
The study notes that excess mortality among younger veterans may be linked to risk-taking behavior, such as substance abuse, not wearing seat belts, or driving under the influence. Difficulty transitioning from military to civilian life may also play a role, since this difficulty is associated with risk-taking, PTSD, anger and poor impulse control. What experts need to better understand, said Howard, is how these problems may be exacerbated by exposure to combat injury, particularly TBI, as well as by broader societal issues such as the opioid crisis.
“What’s happening isn’t happening in a vacuum,” he said. “What this study points to is that when you put all these factors together with additional trauma exposures, it leads to individuals being at increased risk for accidents and exposure to violence.”
- Bilmes LJ. The Long-Term Costs of United States Care for Veterans of the Afghanistan and Iraq Wars. 20 Years of War: A Costs of War Research Series. Brown University. https://watson.brown.edu/costsofwar/files/cow/imce/papers/2021/Costs%20of%20War_Bilmes_Long-Term%20Costs%20of%20Care%20for%20Vets_Aug%202021.pdf
- Stewart IJ, Sosnov, JA.; Howard JT.; Orman JA.; et al. Retrospective Analysis of Long-Term Outcomes After Combat Injury: A Hidden Cost of War. Circulation. Published November 2, 2015. DOI: 10.1161/CIRCULATIONAHA.115.016950.
- Howard, JT; Stewart, IJJ.; Amuan M; Janak JC; Pugh MJ. Association of Traumatic Brain Injury With Mortality Among Military Veterans Serving After September 11, 2001. JAMA Network Open. Published February 11, 2022. DOI: 10.1001/jamanetworkopen.2021.48150.

