WASHINGTON — Part of the VA MISSION Act of 2018 required VA to conduct a nationwide audit of its healthcare system’s capacity, identify gaps in care and make recommendations for modernizing or realigning VA facilities to fill those gaps.
At the end of January, the VA secretary was required to pass VA’s recommendations on to the Asset and Infrastructure Review (AIR) Commission–a group of appointed officials who will take that data and create a report that could help determine where the department’s physical footprint grows and shrinks over the next decades.
A VA Office of the Inspector General (OIG) report calls into question, however, the accuracy of VA’s data when it comes to measuring the department’s capacity to provide specialty healthcare and how inaccurate data might undermine the audit and the MISSION Act’s goals.
During VA’s market assessments in preparation for the AIR Commission recommendations, agency leaders interviewed more than 1,800 VA officials at facilities nationwide to gain an understanding of market trends and relied on those officials to provide accurate data. OIG’s audit came on the heels of those interviews.
“Given the broad scope of these market assessments, the [OIG] team evaluated the risk that major data elements would be materially incorrect and could affect the MISSION Act modernization or realignment recommendations,” the OIG’s December report states.
The auditors focused on specialty care, because there was a higher likelihood that the data would be incorrect. While a metric such as inpatient capacity is relatively simple to calculate using a beds-day of care measurement, specialty care is measured using CPT codes.
“That [specialty care] workload is more difficult to measure, because the information is captured through a complicated coding process that requires the providers to thoroughly document the care provided in the associated medical records,” OIG investigators concluded. “Most outpatient specialty encounters are not reviewed for coding accuracy because checking the coded encounters for errors is labor-intensive.”
Based on a sample of CPT codes assigned to 868 patient counters spread over 12 specialties from 10 randomly selected VA facilities, investigators found that 47% of them were incorrectly coded. As a result, VHA’s reported FY2019 workload numbers for specialty care across all VA care providers was estimated to be overstated by 10.7%. That is the equivalent of 563 full-time specialty care physician positions.
Overstated Workload
“The overstated workload varied based on physician specialties from the equivalent of as few as 369 cardiologists to as many as 727 infectious disease physicians,” the report explains. “This overstatement of workload could result in an inefficient use of VA funds and diminish access to care for veterans if it leads VA officials to place staffing resources where they are not needed.”
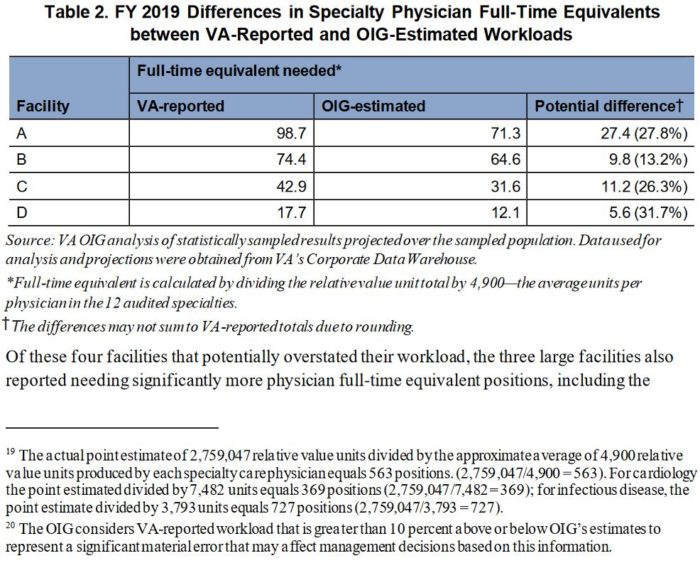
Of the 10 facilities sampled by the OIG, the overestimation was primarily contained in four of them. The largest of these four facilities reported that it needed the equivalent of 98.7 physicians, where the OIG estimated it actually required 71.3, resulting in a 27.8% overestimation. The smallest facility reported a 17.7 physician need, with the audit showing 12.1—a 31.7% overestimation.
The audit also found some inaccuracy regarding patient wait times, but the numbers were small enough that the team found it unlikely to affect VA’s AIR Commission recommendations.
If VA’s market assessment is to accurately identify gaps in the department’s ability to provide healthcare, it will require a higher accuracy of data, investigators stated.
“Without a clear understanding of the work performed, VHA cannot be assured that management decisions at the facility and higher levels are based on verifiable, documented services provided,” the investigators concluded.
Investigators noted that this is not as big a problem for the individual facilities as it is for VHA nationally. Medical facility leaders were aware that specialty physicians did not always choose the most appropriate code and have accounted for that when making staffing changes.
However, the historical codes were not updated, and therefore workload calculations made at the national level were inaccurate
When presented with the inaccuracies, VHA staff told OIG investigators that they would be relying on bed-days of care and the numbers of veterans assigned to each physician for making its initial recommendations to the AIR Commission. Investigators noted in the report, however, that it seems likely that specialty care will become a factor in VA’s conversations with the AIR Commission in the future and that VA leaders will need to ensure that the data they’re working from is accurate.