NORTH HILLS, CA — The last 20 years have brought dramatic changes to the treatment of age-related macular degeneration (AMD) and made early detection more important than ever. For patients with AMD, diagnosis before their vision deteriorates dramatically improves outcomes. In addition, early intervention can halt or slow development of the disease.
“Data show us that treated patients have better vision than those untreated and baseline [visual acuity] at the start of treatment is the best predictor for final measure,” said Steve Ferrucci, OD, FAAP, chief of Optometry, Sepulveda VA, North Hills, Calif., in a National Institutes of Health and National Eye Institute-sponsored presentation. “However, multiple studies tell us that patients are diagnosed with AMD too late.”1
Often patients with early-stage AMD have no symptoms or are unaware that the changes in vision that they are experiencing indicate a problem. The American Academy of Ophthalmology (AAO)’s Age-Related Macular Degeneration Preferred Practice Pattern recommends taking a comprehensive history that includes asking about symptoms of AMD that patients may have dismissed as just a function of aging, such as intermittent or permanent eye floaters or flashes, blind spots or areas of blurriness in otherwise normal vision, spots of flickering light, difficulty seeing at night or in dim light or adjusting between bright and dim light, and seeing straight lines as wavy.
Determining whether a patient has AMD and the stage of disease is critical to management and preservation of vision. “The bottom line is we need to do better in diagnosing AMD earlier, especially wet AMD, and making sure those that need treatment receive it promptly, added Ferrucci. “Time is vision.”
After a thorough history, diagnosis requires several types of assessment. “Macular degeneration treatment depends on its stage and type. Patients with macular degeneration can benefit from a comprehensive eye exam, with evaluation and interventions to mitigate risk factors for progression,” Gina Jackson, VA spokesperson, told U.S. Medicine.
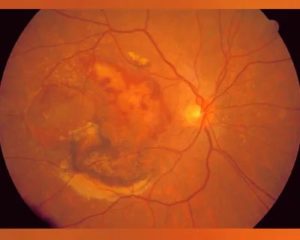
As part of a comprehensive exam, the AAO recommends use of the Amsler grid to identify metamorphopsia, a visual distortion that causes straight lines to appear curved or wavy, and stereoscopic biomicroscopic examination of the macula to detect clinical signs of choroidal neovascularization (CNV) characteristic of wet AMD. These include small hemorrhages, hard exudates, subretinal fluid, macular edema, subretinal fibrosis and pigment epithelial elevation.
Diagnostic Tests

Deb Rock (right), nurse manager for La Crosse Outpatient Clinics, and Cynthia Lang (left), telehealth clinical technician, SFT preceptor and CVT preceptor.at the Tomah, WI, VAMC with equipment used to detect age-related macular degeneration. Photo from Sept. 9, 2020 VAntage Point blog.
Diagnostic tests may include optical coherence tomography (OCT) to determine the presence of subretinal and intraretinal fluid and retinal thickening and optical coherence tomography angiography (OCTA) to assess the retina and choroidal vasculature.
“In addition to an eye examination, intravenous dyes may be injected to help the eye doctor visualize areas of swelling and bleeding inside the eye,” added Jackson. Dyes are used intravenous fundus fluorescein angiography, which can help identify the cause of new symptoms, provide additional information to clarify clinical findings, assess CNV, and monitor response to treatment.
Fundus photography and fundus autofluorescence can also be used in diagnosis and as baseline assessments of AMD. Indocyanine green angiography is sometimes used to enable visualization of the choroidal circulation.
Increasingly, tests of dark adaptation may also be used for diagnosis of AMD and to identify patients with subclinical disease who should be assessed more often. The rod intercept time is the number of minutes the eye requires to adapt from bright light to darkness. This functional test identifies AMD before drusen or macular changes appear.
“Delayed rod-mediated dark adaptation in older adults in normal macular health is associated with incident early AMD three years later, and thus is a functional biomarker for early disease,” researchers led by Cynthia Owsley, PhD, MSPH, Nathan E. Miles Chair, professor, and director of the Clinical Research Unit in the Department of Ophthalmology, Heersink School of Medicine at the University of Alabama at Birmingham and member of the VA’s Center for Visual & Neurocognitive Rehabilitation National Advisory Board, found. “The biological relevance of this test is high, because it assesses translocation of vitamin A derivatives across the retinal pigment epithelium and Bruch’s membrane, two tissues with prominent age- and AMD-related pathology.”2
Early Intervention
While there are no treatments for any stage of dry AMD, a number of interventions can slow progression. More frequent exams can also catch worsening vision or development of wet AMD at its earliest stage.
Ferrucci and his co-authors of Practical Opportunities in AMD Management recommended that “treatment of AMD should be initiated at first detection, regardless of the stage.” Interventions they recommended for all stages of AMD include smoking cessation programs, nutritional supplementation, retinal protection from UVA and UVB light, diet and exercise, and systemic disease management.
The Age-Related Eye Disease Study (AREDS) and AREDS2 studies showed a “specific combination of vitamins including lutein and zeaxanthin could help slow the progression and reduce the risk of vision loss in those patients with intermediate or worse AMD by approximately 25%,” Ferrucci said. Other ingredients in the AREDS2 formula include vitamin C, vitamin E, zinc and copper. In addition to supplements, a diet rich in dark green leafy vegetables, yellow and orange fruits and vegetables that have natural carotenoids, fish high in omega-6 fatty acids such as tuna and salmon, and citrus fruits is recommended.
The American Macular Degeneration Foundation (AMDF) risk factors for AMD include being overweight or having unchecked heart disease or high blood pressure, making improving cardiovascular health particularly important. Physical exercise has also been shown to significantly reduce the risk of AMD and the severity of macular degeneration in individuals with AMD.
Patients should also begin daily or weekly self-screening for progression. The Amsler chart, which resembles graph paper, is the classic home screening tool. The ForeseeHome Monitor has become another common way to detect the metamorphopsia that indicates wet AMD. A number of mobile apps have also entered the space, including SightBook, which can identify visual distortions caused by retinal changes, low light visual acuity, visual acuity, contrast sensitivity and other components of visual health.
- nAMD and RVO: Understanding the Impact on Patient Lives and the Need for Timely Diagnosis and Referral. Eye Health Academy. March 2021.
- Owsley C, McGwin G Jr, Clark ME, et al. Delayed Rod-Mediated Dark Adaptation Is a Functional Biomarker for Incident Early Age-Related Macular Degeneration. Ophthalmology. 2016;123(2):344-351. doi:10.1016/j.ophtha.2015.09.041