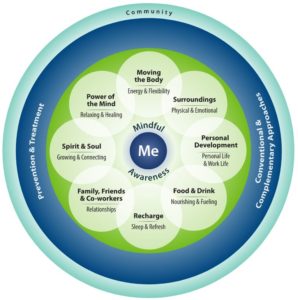
Click To Enlarge: Understanding the Circle of Health
Taking stock of where you are in each of these areas and thinking about where you want to be, is the first step in living a healthier life.
WASHINGTON — For more than a decade, VA has been shifting to a patient-centered model of care, one where providers work together to get a fuller picture of a patient’s life and health. With its Whole Health approach, VA is taking that transformation several steps further.
“Our definition of Whole Health is that it’s an approach to care that empowers and equips veterans to take charge of their health and to live their life to the fullest,” explained Benjamin Kligler, MD, MPH, executive director of VA’s Office of Patient Centered Care and Cultural Transformation. “It takes the focus off what’s the matter with you, which is what healthcare systems have been solely focused on, to what matters to you. What’s important in your life? What’s giving your life meaning? How can we help you access that?”
For patients and for providers, this involves a mental repositioning of how healthcare fits into a person’s life, as well as how patients interact with a healthcare system. In simplified terms, the goal is for veterans and providers to think about how VA can help veterans even when they’re healthy.
“VA has been absolutely outstanding in what healthcare systems typically do—disease-oriented care,” Kligler said. “We identify and manage diseases. We also work toward prevention of those diseases. VA has great outcomes in that area. [The Whole Health approach] is saying that we’re going to continue to do that but expand the picture of what we can do. How can we think a little bit bigger? And put those diseases in the context of the person and what matters most of them. We can be more successful in managing diseases and health problems if we help people be empowered to make change themselves. What are you looking forward to in your life to take that medication, eat right, move more, make social connections?”
To accomplish that, VA is creating new ways for veterans to tap into VA care. The first is a peer-to-peer initiative that VA calls “the Pathway.”
“Veterans get to meet with a fellow veteran [who has] been trained as a Whole Health partner or peer facilitator. They’re trained to start that conversation with the veteran,” Kligler explained. “What’s most important to you in your life right now? They help them look at all the different domains in their life where they could be already strong or where they might need help? What they’re eating, exercise, social connections, spiritual life.”
Veterans also can be exposed to the Whole Health approach through the more traditional method of talking with their clinical provider.
“Now part of what that clinician is talking about is what’s important in your life right now,” Kligler said. “[VA is undertaking] a gigantic training program where we’re reaching out to clinical staff to help them expand their lens.”
That training program is in its early stages, and Kligler estimates it will be two or three years before it’s complete.
Complementary Health
Veterans also can learn about Whole Health by taking classes, working with peers or health coaches and exploring VA’s selection of complementary health programs, such as yoga, tai chi and meditation, as well as nutrition and fitness.
“We’re finding a lot of veterans coming into Whole Health because a buddy told them about a tai chi class,” Kligler said.
Kligler’s own focus on complementary therapies extends back to college when he developed an interest in natural medicines and approaches to health beyond conventional care. Over his 20 years as a primary care physician, he trained in acupuncture, hypnotherapy and herbal medicines and conducted research into delivering complementary therapies to patients, especially those underserved by modern healthcare systems. It was this background that earned him the job as the director of VA’s Integrative Health Coordinating Center and eventually chief of its Whole Health program.
“VA is really out in front in terms of healthcare systems [embracing] complementary medicine,” he said. “We’re the first healthcare system in the country that’s offering as part of medical benefits the range of evidence-based complementary therapies that we offer.”
“There’s still a decent amount of resistance from certain conventional medical people,” he added. “People who haven’t had the opportunity to really explore the good evidence that’s emerged from these things. But the demand from veterans is massive. We get these stories back from veterans [about how these therapies] are helping with pain, anxiety and having more well-being in their life.”
A recent analysis by VA found that 7.8% of enrolled veterans are using some kind of Whole Health service. While that may seem like a small proportion, it represents 500,000 veterans.
“What that says to me is the demand is there and the interest and need from veterans is there.”
The challenge now for Kligler and VA’s Whole Health approach is finding ways to make veterans aware of the full range of services VA offers as early in their post-service life as possible.
“Even while they’re on active duty, but certainly before they leave,” Kligler said. “One of the bits of the [recently-passed Hannon Act] that we’ve been involved with is how to be more visible as part of transition. Whole Health helps give meaning and purpose. So much of leaving the service is ‘I have to find my own purpose.’ [We can] step up to provide tools for people to do that.”
