Click to Enlarge: AUROC for Models Predicting SARS-CoV-2–Related Death Among 7.6 Million Veterans Affairs Enrollees Compared With Age-Based Allocationa
SEATTLE — A model developed by VA researchers showed promise for preventing a substantial number of SARS-CoV-2-related deaths during vaccine rollout, if used in the general population, according to a new study.
Based on 7.6 million enrollees in VHA, a logistic regression model (COVIDVax) was developed to estimate risk of COVID-19–related death using 10 characteristics:
- sex,
- age,
- race,
- ethnicity,
- body mass index,
- Charlson Comorbidity Index,
- diabetes,
- chronic kidney disease,
- congestive heart failure and
- the Care Assessment Need score.
Researchers from the VA Puget Sound Healthcare System and the University of Washington, both in Seattle, estimated that the model would save more lives than prioritizing vaccination based on age or on the national Centers for Disease Control and Prevention vaccination allocation, recommended by its Advisory Committee on Immunization Practices.
Essentially, the authors argued that a strategy that prioritizes individuals for SARS-CoV-2 vaccination according to their risk of mortality from the infection would help minimize deaths during vaccine rollout.
Their prognostic study, published in JAMA Network Open, used data from more than 7.6 million veterans enrolled in the VA healthcare system as of May 21, 2020, to develop and internally validate a logistic regression model (COVIDVax) that predicted 2,422 SARS-CoV-2-related deaths during the observation period from May 21 to Nov. 2, 2020. Researchers extracted information on baseline characteristics known to be associated with SARS-CoV-2–related mortality, from the VA electronic health records.
Risk scores were developed for all current VA enrollees, who were 92.4% men and had a mean age of 66.2; most, 64%, were white, with 14.6% Black and 5.2% Hispanic enrollees.
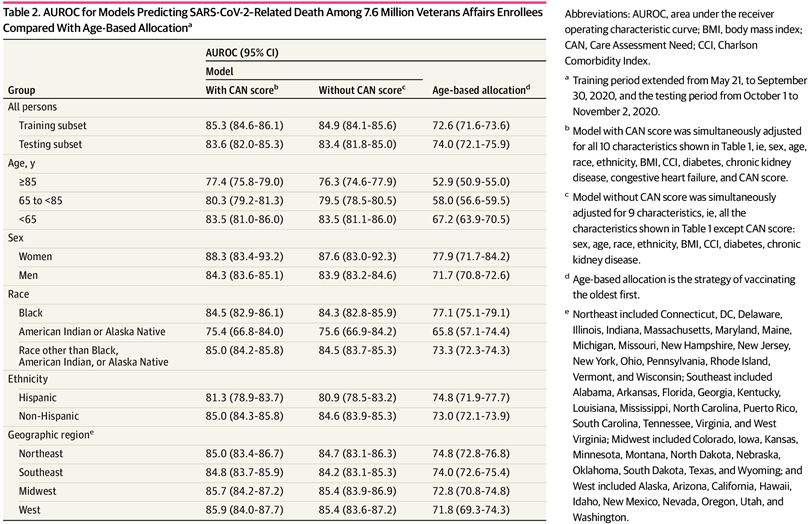
From a starting pool of 16 potential predictors, 10 were included in the final COVIDVax model (listed above) and “exhibited excellent discrimination with area under the receiver operating characteristic curve (AUROC) of 85.3% (95% CI, 84.6%-86.1%), superior to the AUROC of using age alone to stratify risk (72.6%; 95% CI, 71.6%-73.6%). Assuming vaccination is 90% effective at preventing SARS-CoV-2–related death, using this model to prioritize vaccination was estimated to prevent 63.5% of deaths that would occur by the time 50% of VA enrollees are vaccinated, significantly higher than the estimate for prioritizing vaccination based on age (45.6%) or the US Centers for Disease Control and Prevention phases of vaccine allocation (41.1%),” according to researchers.
Herd Immunity
Basically, they concluded that the COVIDVax model could prevent a large proportion of deaths expected to occur during vaccine rollout before sufficient herd immunity is achieved.
The authors estimated that, by the time 50% of the population was vaccinated, prioritizing vaccinees based on the model would result in 22.4% fewer SARS-CoV-2-related deaths than an approach based on CDC-ACIP allocation phases and 17.9% fewer deaths than an approach based on age alone, explaining, “Our findings suggest that healthcare systems, such as VA, that have the capability to do so should consider implementing our model, and the CDC-ACIP should consider modification or substratification of their proposed allocation phases to better capture risk of SARS-CoV-2-related mortality.”
In fact, they pointed out that their model demonstrated high sensitivity for SARS-CoV-2-related death even at low levels of vaccination. That means substantial reductions in SARS-CoV-2–related mortality even after small proportions of the population have been vaccinated, they suggested.
“The actual numbers of deaths prevented would be greater the longer it takes to vaccinate and the higher the absolute death rate without vaccination,” the study team wrote. “For example, if it takes 150 days to vaccinate 50% of VA enrollees, in whom approximately 20 deaths per day were occurring at baseline, then 3,000 (150 × 20) deaths would occur without vaccination, 1,905 deaths (63.5%) would be prevented by COVIDVax-based vaccination, but only 1,233 (41.1%) would be prevented by CDC-ACIP phased allocation. Alternatively, if it takes 200 days to vaccinate 50% of VA enrollees and the baseline mortality is higher at approximately 30 deaths per day (given the surge in SARS-CoV-2-related mortality since the study’s observation period), then 6,000 (200 × 30) deaths would occur without vaccination, 3,810 (63.5%) would be prevented by model-based vaccination and 2,460 (41.1%) by CDC-ACIP phased allocation.”
In light of that, the researchers prevented their best case for using a mortality-risk-based model to roll out vaccine programs. The study was accepted in February and published in April.
“Given that more than 2,500 SARS-CoV-2-related deaths per day have been reported in the United States since Dec. 15, 2020, and that vaccination rollout has been slower than expected, a very large number of deaths can be prevented by strategies that directly model and prioritize high-risk persons,” they argued.
- Ioannou GN, Green P, Fan VS, et al. Development of COVIDVax Model to Estimate the Risk of SARS-CoV-2–Related Death Among 7.6 Million US Veterans for Use in Vaccination Prioritization. JAMA Netw Open. 2021;4(4):e214347. doi:10.1001/jamanetworkopen.2021.4347

