PITTSBURGH — Mortality rates are lower for veterans who receive all of their post-kidney transplant care within the VHA than those who receive care outside the VA through Medicare coverage, according to a recent study.
The results are especially important, because implementation of the MISSION Act likely means more VHA patients will be receiving their care outside of that system, according to the authors from the VA Pittsburgh Healthcare System and the University of Pittsburgh School of Medicine.
The report in the Clinical Journal of the American Society of Nephrology pointed out that little information was available on whether transplant-related care provided after a kidney transplant is of equal quality through the different healthcare systems. It noted that many kidney transplant recipients enrolled in the VHA also are enrolled in Medicare and eligible to receive both VA and private sector care.1
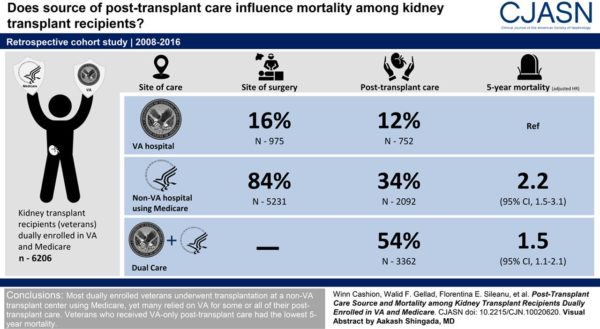
To look at where care is received and how that affects mortality, the research team conducted a retrospective cohort study of veterans who underwent kidney transplantation between 2008 and 2016 and were dually enrolled in VHA and Medicare at the time of surgery.
The 6,206 veteran patients were categorized on the basis of the source of transplant-related care—i.e., outpatient transplant visits, immunosuppressive medication prescriptions, calcineurin inhibitor measurements—delivered during the first year after transplantation at either VHA only, Medicare only or dual care, defined as mixed use of VHA and Medicare.
With 16% of patients undergoing transplantation at a VHA hospital and 84% doing so at a non-VA facility using Medicare, post-transplant care was received by 12% through VHA only, 34% through Medicare only and 54% through dual care, according to the study.
Researchers reported that, compared with patients who were VHA-only, five-year mortality was significantly higher among patients who were Medicare-only (adjusted hazard ratio, 2.2; 95% confidence interval, 1.5 to 3.1) and patients who were dual care (adjusted hazard ratio, 1.5; 95% confidence interval, 1.1 to 2.1).
“Most dually-enrolled veterans underwent transplantation at a non–Veterans Health Administration transplant center using Medicare, yet many relied on Veterans Health Administration for some or all of their post-transplant care,” the authors concluded. “Veterans who received Veterans Health Administration-only post-transplant care had the lowest five-year mortality.”
Post-Transplant Care
“Our findings indicate that veterans who receive all their post-transplant care within the VA have the lowest long-term mortality,” added lead researcher Steven D. Weisbord, MD, MSc. “The results are very important in light of the fact that, with the MISSION Act, many more veterans will now have the option of receiving their post-transplant care outside the VA in the private sector.”
The study did not explain why mortality rates are different, although the authors posited that the quality of post-transplant care could be higher within the VA, or VA Transplant Centers might require a more-arduous evaluation process that results in the selection of healthier transplant recipients or donor organs.
An accompanying editorial described how the VA has a well-established national transplant program which provides a standardized electronic process to facilitate veteran referral to one of seven VA kidney transplant centers and to optimize the delivery of post-transplant care within the system.2
The commentators, Namrata Krishnan, MD, MBBS, and Susan T. Crowley, MD, MBA, both of the VA Connecticut Healthcare System in West Haven, CT, and Yale University in New Haven, CT, wrote, “Despite criticism regarding limited geographic accessibility and living-donor transplant rate, 19% of veterans receive their kidney allograft via a VA transplant center, with the remainder accessing community-based transplant services. New legislation expanding V payment authority for community health care services, combined with the VA’s establishment of shared-care transplant arrangements with select academic affiliates, will further extend veterans’ choices for how transplant care services may be received This expanded mento of transplant care delivery options may heighten the complex interactions between site of care and payor and potentially cause fragmentation of care with adverse health outcomes. Hence, it is imperative to better characterize veteran patient choices related to site of care and pay, and the effect those choices have on kidney transplant outcomes.”
Background information in the article recounted how, in 2014, the Congress passed the Veterans Access, Choice and Accountability Act to expand options for veterans to receive care outside the VA. While that legislation resulted in relatively limited utilization of private sector care, as decisions authorizing non-VA care rested primarily with VA personnel, the system changed in 2019 with implementation of the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSIONs) Act. The MISSION Act increased the number of veterans eligible for non-VA care, and shifted decisions on the location of care primarily to veterans.
- Cashion W, Gellad WF, Sileanu FE, Mor MK, Fine MJ, Hale J, Hall DE, Rogal S, Switzer G, Ramkumar M, Wang V, Bronson DA, Wilson M, Gunnar W, Weisbord SD. Source of Post-Transplant Care and Mortality among Kidney Transplant Recipients Dually Enrolled in VA and Medicare. Clin J Am Soc Nephrol. 2021 Mar 8;16(3):437-445. doi: 10.2215/CJN.10020620. Epub 2021 Feb 18. PMID: 33602753.
- Krishnan N, Crowley ST. Post-Kidney Transplant Care and Health Outcomes of US Veterans. Clin J Am Soc Nephrol. 2021 Mar 8;16(3):337-339. doi: 10.2215/CJN.00580121. Epub 2021 Feb 18. PMID: 33602754.