Crohn’s, Colitis Patients Have Generally Higher Infection Risks
ANN ARBOR, MI — The lack of continuity of care among VA patients with inflammatory bowel disease (IBD) is associated with poor outcomes, such as disease flares requiring corticosteroid treatment, hospitalization and surgical intervention.
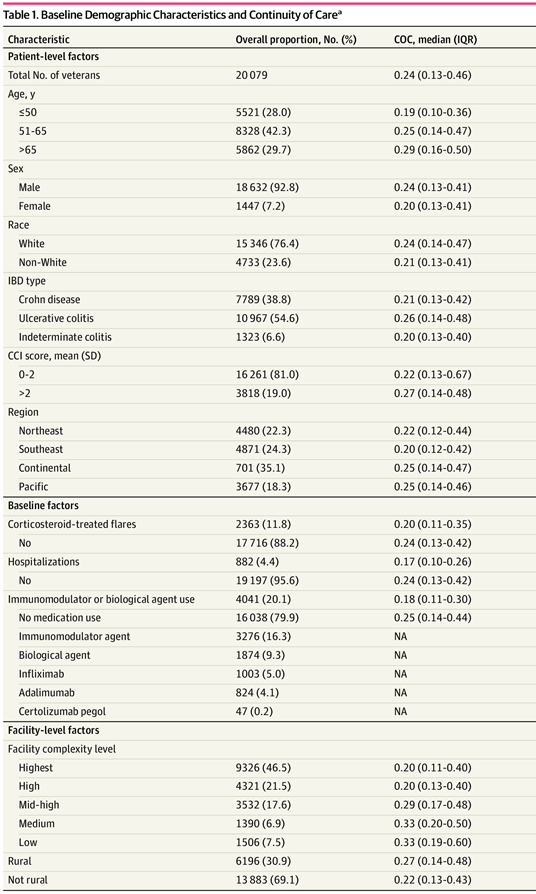
That’s according to a cohort study of 20, 079 veterans with IBD, led by researchers from the Ann Arbor, MI, VA Health System and the University of Michigan. The study team also found significant variation in continuity of care for those patients.
Their report in JAMA Network Open raised concerns about the lack of consistency in an integrated system with systematically enhanced care coordination. The report also questioned whether care coordination was a problem for other VA patients with complex chronic conditions.
“Our findings show that continuity of care is highly variable across patients with IBD,” wrote lead author Shirley Ann Cohen-Mekelburg, MD, MS, who is affiliated with both the VAMC and the university. “The prevalence of low continuity of care in IBD is likely multifactorial and may relate to factors like a lack of provider accountability, less focus on coordinating specialty care and poor patient access to gastroenterologists.”
Cohen-Mekelburg suggested that barriers to collaborative care need to be better evaluated, explaining, “We need, for example, to provide PCPs and gastroenterologists with better communication and coordination resources when managing IBD patients. This is hugely important.”
The study pointed out that healthcare fragmentation is associated with inefficiency and worse outcomes. Continuity of care models were developed to address fragmentation.
The VHA Corporate Data Warehouse was used to identify veterans with IBD who received care in healthcare system between Jan. 1, 2002, and Dec. 31, 2014. Included patients were veterans with IBD who had a primary care physician and at least four outpatient visits with key physicians—gastroenterologist, primary care physician, and surgeon—within the first year after an index IBD encounter. Data were analyzed from November 2018 to May 2020.
Among the 20,079 veterans with IBD who met the inclusion criteria, most, 92.8%, were men, and the median age was 59. Researchers reported that, in the first year of follow-up, substantial variation in the dispersion of care was observed (median [IQR] COC, 0.24 [0.13-0.46]). They determined that a low level of COC was associated with a higher likelihood of outpatient flares that required:
-
corticosteroids (adjusted hazard ratio [aHR], 1.11; 95% CI, 1.01-1.22),
-
hospitalizations (aHR, 1.25; 95% CI, 1.06-1.47), and
-
surgical interventions (aHR, 1.72; 95% CI, 1.43-2.07).
Over Years 2 and 3 of follow-up, 4,658 patients (23.2%) had an outpatient flare, 2,068 (10.3%) required hospitalization, and 943 (4.7%) required a surgical procedure, according to the article.
“Results of this cohort study showed a wide variation in dispersion of IBD care and an association between a lower level of COC and active IBD and worse outcomes,” the authors wrote. “The findings suggest that investigating the barriers to COC in integrated systems that have invested in care coordination is key to not only better understanding COC but also identifying opportunities to improve care fragmentation.”
Infection Double Whammy
Lack of continuity of care can be especially dangerous for IBD patients in the current environment, according to other researchers, because many IBS patients have a double whammy when it comes to infections. They have impaired immune systems related to their diseases, and many of them also are being treated with immunosuppressive medications.
The new study in the Journal of Crohn’s & Colitis examined how effective pneumococcal vaccination is in protecting against severe pneumococcal disease in a population of older, mostly male patients.2
Researchers from, the William Jennings Bryan Dorn VAMC and the University of South Carolina College of Pharmacy both in Columbia, and colleagues pointed out that streptococcus pneumoniae is an important pathogen responsible for severe pneumococcal diseases, including pneumonia, bacteremia/sepsis and meningitis.
The study team identified patients with IBD and SPD from the VA Health Administration database, using ICD9/10 codes. They gathered information on pneumococcal vaccination and use of immunosuppressant medications, while also taking into account demographics, medications, vaccination and comorbidities.
Ultimately, the authors identified 1,798 cases of SPD—283 pneumonia, 1,513 bacteremia, and 2 meningitis. They determined that SPD patients were older—60.9 years vs. 59.4 years; p<0.001—and, had more comorbidities (Charlson Comorbidity Index of 2.11 vs. 0.96; p<0.001). Those patients also had increased likelihood of mortality (4.6% vs. 1.5%, p<0.001), according to the report.
Results indicate that the risk of SPD was increased in Crohn’s disease (HR 1.15; 95% CI 1.05-1.27) and with more comorbidities (HR 1.45; 95% CI 1.42-1.48). Furthermore, researchers emphasize that use of immunosuppressive medications increased the risk of SPD.
On the other hand, receipt of PCV13 either alone or in combination with PPSV23 predicted a fivefold decreased risk of SPD compared with no vaccination, they write.
“Vaccination with PCV13 alone or in combination with PPSV23 and revaccination with PPSV23, was protective against SPD,” the authors conclude. “All IBD patients should be evaluated for pneumococcal vaccination, particularly those receiving or expected to receive immunosuppressive therapies.”
The VA has reported that it provides the pneumococcal vaccine to almost 95% of veteran patients recommended to receive it.
In light of the documented higher infection risks, a study earlier this year sought to determine whether veterans with IBD were also at greater risk of COVID-19 but found that was not the case.
The research led by the Corporal Michael J. Crescenz VAMC in Philadelphia and published in the American Journal of Gastroenterology noted little data on whether patients with IBD have an increased risk of developing SARS-CoV-2 compared with patients without IBD.3
The study team conducted a nationwide retrospective cohort study at the VA from Jan. 1, 2020, to June 30, 2020. Each veteran with IBD was matched with two patients without IBD on age, sex, race, location and comorbidities. The outcome of interest was development of SARS-CoV-2.
Results indicated that, among 38,378 patients with IBD and 67,433 patients without IBD, 87 (0.23%) and 132 (0.20%) patients developed incident SARS-CoV-2 infection, respectively (P = 0.29).
“Patients with IBD are not at a significantly increased risk of developing SARS-CoV-2 infection when compared with patients without IBD,” the authors concluded.
- Cohen-Mekelburg S, Saini SD, Krein SL, et al. Association of Continuity of Care With Outcomes in US Veterans With Inflammatory Bowel Disease. JAMA Netw Open. 2020;3(9):e2015899. doi:10.1001/jamanetworkopen.2020.15899
- Love BL, Finney CJ, Gaidos JKJ. Effectiveness of Conjugate and Polysaccharide Pneumococcal Vaccines for Prevention of Severe Pneumococcal Disease Among Inflammatory Bowel Disease Patients. J Crohns Colitis. 2021 Jan 25:jjab017. doi: 10.1093/ecco-jcc/jjab017. Epub ahead of print. PMID: 33491047.
- Khan N, Patel D, Xie D, Pernes T, et. Al. re Patients With Inflammatory Bowel Disease at an Increased Risk of Developing SARS-CoV-2 than Patients Without Inflammatory Bowel Disease? Results From a Nationwide Veterans’ Affairs Cohort Study. Am J Gastroenterol. 2020 Oct 19. doi: 10.14309/ajg.0000000000001012. Epub ahead of print. PMID: 33079751.