DALLAS – Use of direct-acting antiviral therapy to essentially cure hepatitis C virus does not completely eliminate the risk of developing hepatocellular carcinoma, but recent studies suggest it can significantly reduce mortality rates.
The 15% to 20% of HCV patients who develop cirrhosis of the liver still have a 1% to 5% annual risk of developing HCC, according to the national Centers for Disease Control and Prevention. And that doesn’t disappear for patients who achieve sustained virologic response (SVR).
A report late last year in the journal Gastroenterology noted a controversy over the benefit of DAA therapy for HCV in patients with a history of liver cancer. A study led by University of Texas Southwestern Medical Center researchers in Dallas and including participation from the VA Puget Sound Healthcare System in Seattle, WA, and the McGuire VAMC, in Richmond, conducted a multicenter cohort study to compare overall survival between patients with HCV infection treated with DAAs and patients who did not receive DAA treatment for their HCV infection after complete response to prior HCC therapy.1
HCC patients had been treated with resection, local ablation, transarterial chemo- or radioembolization, or radiation therapy, from January 2013 through December 2017 at 31 health care systems throughout the United States and Canada. Researchers advise that, of 797 patients with HCV-related HCC, 383 (48.1%) received DAA therapy and 414 (51.9%) did not receive treatment for their HCV infection after complete response to prior HCC therapy.
Results indicated that, among DAA-treated patients, 43 deaths occurred during 941 person-years of follow-up, compared with 103 deaths during 526.6 person-years of follow-up among patients who did not receive DAA therapy (crude rate ratio, 0.23; 95% confidence interval [CI], 0.16-0.33).
“In inverse probability-weighted analyses, DAA therapy was associated with a significant reduction in risk of death (hazard ratio, 0.54; 95% CI, 0.33-0.90),” the authors wrote. “This association differed by sustained virologic response to DAA therapy; risk of death was reduced in patients with sustained virologic response to DAA therapy (hazard ratio, 0.29; 95% CI, 0.18-0.47), but not in patients without a sustained virologic response (hazard ratio, 1.13; 95% CI, 0.55-2.33).”
The study concluded that “DAA therapy was associated with a significant reduction in risk of death.”
A real-world cohort study published this summer in Cancer Management and Research bolstered those findings.2
“Hepatocellular carcinoma (HCC) caused by hepatitis C virus (HCV) infection has become less and less due to the use of direct-acting antiviral agents (DAAs),” Chinese researchers pointed out. “Although it may be common to assume that eradication of the virus should improve the survival of HCC patients, large-scale randomized clinical data to support the correlation between viral load and prognosis are still lacking in China. The aim of the study was to evaluate the efficacy of antiviral therapy for HCC patients with active HCV infection.”
To do that, the study team retrospectively enrolled 80 HCC patients with active HCV infection, which was defined as positive for HCV antibody with detectable HCV RNA by polymerase chain reaction.
Researchers reported that 44 patients (55.0%) received interferon combined with ribavirin treatment, and 23 patients achieved sustained virological response.
Survival Rate
“The 1-year survival rate in patients who achieved SVR was the highest, followed by those with non-SVR after antiviral treatment, and those without antiviral therapy (1-year survival rate were 91.3%, 88.4%, and 73.1%, respectively, P = 0.012),” according to the authors.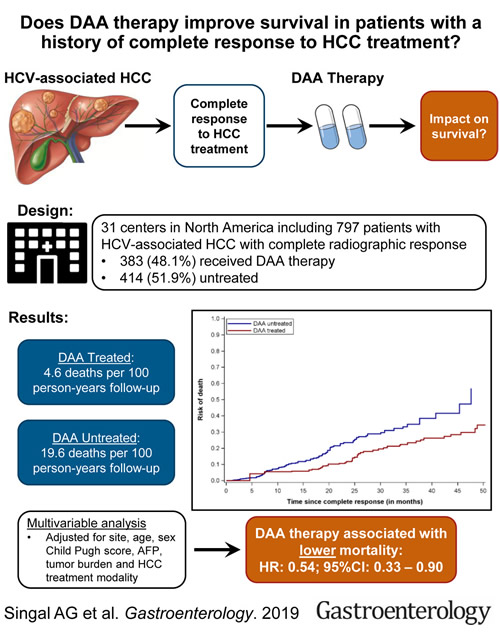 In the univariate analysis, they said, alcohol intake and alpha-fetoprotein >20 ng/mL were associated with lower overall survival (OS) (P = 0.025 and P = 0.044, respectively), while SVR after antiviral treatment was associated with longer OS (P = 0.016), adding that, in the multivariate analysis, only SVR after antiviral treatment was significantly associated with OS (P = 0.014).
In the univariate analysis, they said, alcohol intake and alpha-fetoprotein >20 ng/mL were associated with lower overall survival (OS) (P = 0.025 and P = 0.044, respectively), while SVR after antiviral treatment was associated with longer OS (P = 0.016), adding that, in the multivariate analysis, only SVR after antiviral treatment was significantly associated with OS (P = 0.014).
“Our results ensured that the elimination of HCV substantially improved OS in HCC patients with active HCV infection, and the prognosis of those patients without antiviral therapy was poor,” researchers concluded.
DAA has been used to cure more than 100,000 VA patients of hepatitis C, which is the leading cause of HCC in the United States.
“The risk [of HCC] remains high in patients who have progressed to cirrhosis already,” said Fasiha Kanwal, MD, MSHS, an investigator in the Clinical Epidemiology & Comparative Effectiveness Program at the Center for Innovations in Quality, Effectiveness and Safety at the Michael E. DeBakey VAMC, chief of the Gastroenterology and Hepatology Section at the Baylor College of Medicine, both in Houston, and editor-in-chief of Clinical Gastroenterology and Hepatology when she spoke with U.S. Medicine last year.
The estimate is that 30% to 40% of veterans had already developed cirrhosis when they received treatment for HCV.
With more than 30,000 veterans at elevated risk of HCC, the VA has led national research into the relationship between HCV infection and treatment and development of liver cancer.
“There has been extensive debate about the potential benefit of DAA therapy in patients with a history of HCC, primarily related to concerns about the risk of HCC recurrence,” wrote the authors of the Gastroenterology study. “While recent data have suggested that DAA therapy after complete HCC response does not appear to increase recurrence, to the best of our knowledge our study represents the first to demonstrate a survival benefit of DAA therapy in this patient population.”
Researchers pointed out that HCC treatments such as surgical resection and local ablative therapies, are potentially curative but also are limited by high risk of recurrence, with five-year mortality rates approaching 50%.
The report noted that hepatic decompensation was one of the most common causes of death in patients without SVR but was not observed in any of the four patients with SVR.
“Although DAA therapy was associated with a consistent survival benefit across most patient subgroups, this association was mitigated in those who were treated with TACE, as well as those with HCC recurrence, likely due to a higher risk of HCC mortality,” according to the researchers. “Although DAA therapy can help improve or stabilize liver function in these patients, the high risk of recurrence and persistent HCC-related mortality highlights a continued need for adjuvant therapy after HCC complete response. In the absence of proven adjuvant agents, close surveillance after complete response may increase early tumor detection and minimize HCC-related mortality.”
On the other hand, the authors advised that reductions in mortality were most evident in patients undergoing surgical resection or ablation, which would be less prone to misclassification of complete response.
They added that lack of data on incident development of hepatic decompensation during study follow-up made it impossible to demonstrate that any survival benefit was definitively related to preservation of liver function.
- Singal AG, Rich NE, Mehta N, et al. Direct-Acting Antiviral Therapy for Hepatitis C Virus Infection Is Associated With Increased Survival in Patients With a History of Hepatocellular Carcinoma. Gastroenterology. 2019;157(5):1253-1263.e2. doi:10.1053/j.gastro.2019.07.040
- Luo Y, Zhang Y, Wang D, Shen D, Che YQ. Eradication of Hepatitis C Virus (HCV) Improves Survival of Hepatocellular Carcinoma Patients with Active HCV Infection – A Real-World Cohort Study. Cancer Manag Res. 2020;12:5323-5330. Published 2020 Jul 2. doi:10.2147/CMAR.S254580

