PITTSBURGH—Almost 492,000 women veterans used the VA health care system in fiscal year 2017, a nearly 150% increase since fiscal year 2003, according to VA statistics.
Those numbers are only expected to increase. While the Veteran Population Projection Model 2016, the latest version, predicts that the total number of veterans is expected to decline from 20 million in 2017 to 13.6 million 2037, it also estimates that women will make an increasingly higher percentage of those numbers. The percentage of male veterans is expected to decline 2.3%, while the female veterans are predicted to increase 0.7%, and these numbers will continue to increase in years to come. VA has worked to improve the gender-specific care for this population of veterans, but more work needs to be done.
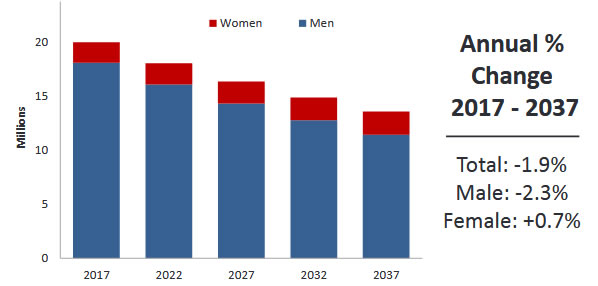
The total Veteran Population is predicted to decline from 20.0 million in 2017 to 13.6 million in 2037
That’s one of the reasons the continuing perception that the VA health system discriminates against women is such a difficult problem. Two recent studies underscored the issue in younger female veterans.

During an award ceremony at Wheeler Army Airfield in Hawaii, Capt. Renee Serell, assigned to 3rd Battalion, 25th Aviation Regiment “Hammerheads” (General Support Aviation Battalion), 25th Combat Aviation Brigade, 25th Infantry Division was awarded the Aeromedical Outstanding Achievement Award from the Society of United States Army Flight Surgeons by Lt. Col. Kacie Lee, commander of 3-25 GSAB during an award ceremony. With increasingly more women at all levels in the military, the VA is struggling with assuring equal and respectful care of female veterans. Army photo by 1st Lt. Ryan DeBooy
A report in the journal Medical Care pointed out, “Experiences of discrimination are associated with poor health behaviors and outcomes. Understanding discrimination in health care informs interventions to improve health care experiences.”1
VA Pittsburgh Healthcare System and University of Pittsburgh-led researchers sought to describe the prevalence of—as well as, variables associated with—perceived gender-based discrimination in VHA facilities. To do that, they conducted a cross-sectional, telephone-based survey of a random national sample of young female veterans aged 18 to 45.
Results demonstrated that, among 2,294 women veterans, 33.7% perceived gender-based discrimination at the VA. That view was most associated with medical illness [adjusted odds ratio (aOR)=1.67, 95% confidence interval (CI)=1.34, 2.08], mental illness (aOR=2.06, 95% CI=1.57, 2.69), and military sexual trauma (aOR=2.65, 95% CI=2.11, 3.32).
On the other hand, receiving most healthcare from the same VA provider (aOR=0.73, 95% CI=0.57, 0.94) and receiving care at a VA site with a women’s health clinic (aOR=0.76, 95% CI=0.61, 0.95) were associated with reduced odds of any perceived gender-based discrimination.
Researchers determined that the 733 women who perceived gender-based discrimination were more likely to:
- Be of increased age,
- Have a medical illness, and
- Have a history of military sexual trauma.
“One-third of women Veterans perceived gender-based discrimination in VA. Obtaining most medical care from the same VA provider and having a women’s health clinic at one’s VA were associated with less perceived discrimination,” the authors concluded.
A study late last year, conducted by the VA Central Western Massachusetts Healthcare System in Leeds, MA, and the University of Massachusetts Medical School in Worcester, was in line with those findings, although it focused on specialty care.
The report in Women’s Health Issues noted, “In the past decade, the U.S. Department of Veterans Affairs (VA) has responded to a dramatic increase in women veterans seeking care by expanding Women’s Health training to more than 5,000 women’s health primary care providers and changing the culture of the to be more inclusive of women veterans. These initiatives have resulted in increased patient satisfaction and quality of care, but have focused mostly on primary care settings. Less is known about women’s experiences in specialty care within VA.”2
To remedy that, researchers conducted a qualitative study to examine women veterans’ experiences with VA specialty care providers, with a focus on cardiovascular, musculoskeletal and mental healthcare settings.
The study team used semi-structured interviews, conducted with 80 women veterans who served during the Iraq and Afghanistan conflicts at four VA facilities nationwide, to better understand women veterans’ experiences with VA specialty care providers, including their perceptions of gender bias.
The authors concluded that four major themes emerged from interviews with the women:
- A perception that that VA specialty care providers listened to them or took their symptoms seriously;
- Reports that patients were told their health conditions or symptoms were attributable to hormonal fluctuations;
- A belief that differences in care based on whether the VA specialty provider was male or female; and
- Recommendations for how gender-sensitive specialty care might be improved.
Touting their study as the first to delve into perceived gender bias experienced by women veterans in VA specialty care, researchers wrote, “Women felt that their symptoms were disregarded or diminished by their specialty care providers. Although women veterans report positive experiences within women’s health clinics and the primary care setting, their negative experiences in VA specialty care suggest that some providers may harbor unintentional or unconscious gender biases.”
Those concerns have been taken up by veterans’ advocacy groups. Testifying last spring before the Subcommittee on Health of the House Committee on Veterans’ Affairs, Kristina Keenan, past-commander of Post 605, the Benjamin Franklin Post of the Veterans of Foreign Wars, pointed out, “VA has worked to improve the gender-specific care for this population of veterans, but more work needs to be done. Women veterans using VA often have complex healthcare needs that require specialty care for service-connected conditions such as post-deployment readjustment challenges, post-traumatic stress disorder due to war-related trauma and sexual trauma, mental health care and substance use disorders—services which, on average, they use at higher rates and more often than male veterans.”
Keenan added, however, “The VFW is disappointed not a single piece of legislation became law in the 115th Congress to address the needs of women veterans. This must change in the 116th Congress.”
- MacDonald S, Judge-Golden C, Borrero S, Zhao X, Mor MK, Hausmann LRM. Experiences of Perceived Gender-based Discrimination Among Women Veterans: Data From the ECUUN Study [published online ahead of print, 2020 Jan 29]. Med Care. 2020;10.1097/MLR.0000000000001304. doi:10.1097/MLR.0000000000001304
- Mattocks K, Casares J, Brown A, et al. Women Veterans’ Experiences with Perceived Gender Bias in U.S. Department of Veterans Affairs Specialty Care [published online ahead of print, 2019 Nov 14]. Women’s Health Issues. 2019;S1049-3867(19)30478-5. doi:10.1016/j.whi.2019.10.003

