Delays in VA Appointments Pose Challenges
SAN ANTONIO, TX — A new program at the Brooke Army Medical Center at Fort Sam Houston aims to give transitioning servicemembers with inflammatory bowel disease the information they need to manage their disease when they leave active duty.
While the educational/behavioral intervention markedly improves patient knowledge of their disease and reduces anxiety, long wait times for post-transition appointments at the VA can complicate care for new veterans with ulcerative colitis or Crohn’s disease.
“Transition from active-duty service to the VA with a chronic disease such as IBD is a time of increased vulnerability and risk for low of continuity of care,” Anish Patel, DO, director of the IBD Center at BAMC and Laurie Keefer, MD, of Mount Sinai Hospital in New York, explained in a presentation at the 2019 AMSUS, The Society of Federal Health Professionals, annual meeting in December.1
To better understand issues faced by transitioning servicemembers, the American College of Gastroenterology provided a grant for Patel and Keefer to research the process and how it might be improved.
The first problem they identified was a “mind-boggling lack of health literacy,” Patel told U.S. Medicine. All the servicemembers took three questionnaires to assess their level of preparedness for transition and ability to advocate for their healthcare, anxiety and depression.
In terms of understanding of their healthcare needs, “the questions were very basic,” Patel said. “We were amazed that it didn’t matter what rank a patient was, from full colonel to 21-year-old private, most didn’t know what disease they had or what drug they were on.”
On a 100-point screening for preparation to take control of their healthcare (TRAQ-5), usually given to assess the ability of teens and young adults to take over their medical care from their parents, the average score was about 60 with just three months to go before the date of transition.
Two Interventions
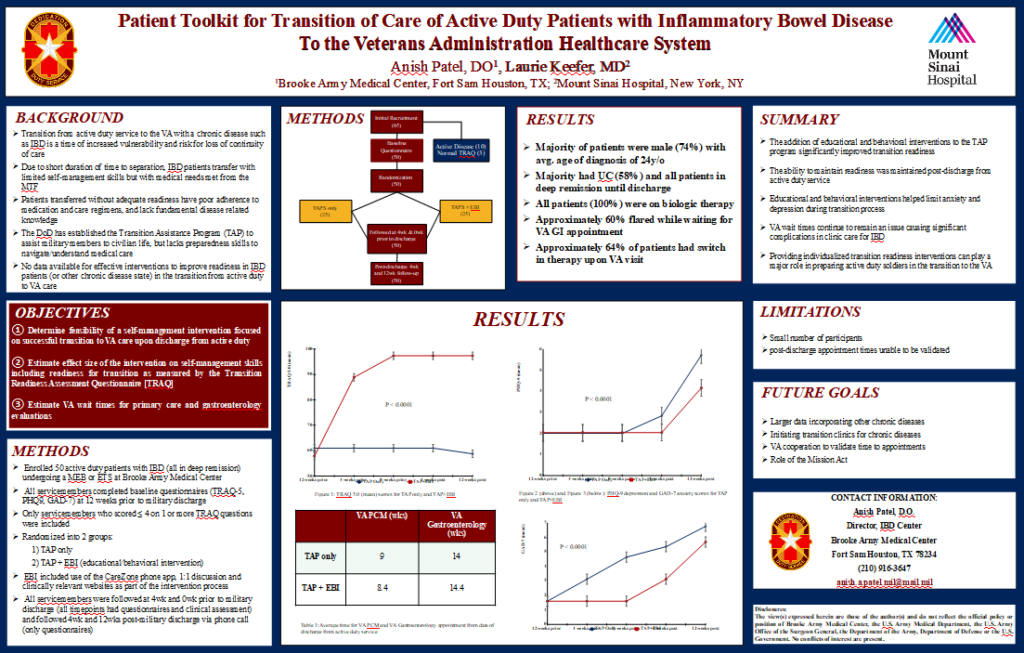
The researchers enrolled 50 active-duty patients with IBD who were transitioning as a result of a Medical Evaluation Board (MEB) or Expiration-Term of Service (ETS). All patients were in deep remission and on biologic therapies.
The study split the servicemembers into two groups. One went through the usual Transition Assistance Program (TAP) offered by the DoD to prepare military members for the adjustment to civilian life and the other participated in TAP as well as an active educational/behavioral intervention.
The 25 patients in the intervention arm received a free commercial phone app called CareZone, which allowed them to enter their doctor’s name, what medications they took, at what dose and how often. They could also take photos of any rashes associated with their disease, such as erythema nodosum, and enter notes on symptoms as well as questions to ask their provider at the next appointment.
In addition, these patients received education on their disease state, along with pictures that illustrated the condition and showed what was affected. A single sheet summarized what they needed to know.
All participants were reassessed four weeks before discharge, at time of discharge, and at four and 12 weeks after discharge.
For servicemembers who received the interventions, TRAQ-5 scores rose to about 80 in the month before discharge and approached 100 at the time of discharge. Individuals who went through TAP only, saw no improvement in their preparation to assume responsibility for their disease management.
After transitioning to veteran status, those who received the intervention also maintained lower scores on their anxiety and depression assessments. “Even when flaring, resilience didn’t wane when they were taught what to do,” Patel noted.
Continue Reading this Article: Post-transition Complications