IOWA CITY, IA–Antibiotics appear to be routinely overprescribed for routine urological procedures within the VHA, according to a new study.
In fact, the drugs were overused in up to 60% of patients undergoing transurethral resection of bladder tumor, transurethral resection of the prostate, and ureteroscopy at five VAMCs in different parts of the United States, an article in JAMA Network Open noted.1
Researchers from the Iowa City, IA, VA and the University of Iowa said that extended use of antibiotics following the procedures was the usual cause of overuse.
While patients undergoing a urological or any other surgical procedure often are prescribed antibiotics as a precaution to prevent a surgery-related infection, overuse can promote antibiotic resistance and put patients at potential harm, such as an increased risk of infection by C. difficile bacteria, the study noted.
The American Urological Association recommends that antibiotics should be given for no more than 24 hours following most urological procedures in the absence of preexisting and untreated bacterial colonization.
“This study shows that antibiotics are often continued for several days after common urologic procedures, even when there is no clear indication for antibiotics. This seemingly unnecessary use of antibiotics is exposing patients to potential harm,” explained co-author Daniel Livorsi, MD, a physician with the Iowa City VA Health Care System and the University of Iowa Health Care system. “Reducing unnecessary antibiotic use in this setting is just one example of how physicians can be better stewards of antibiotics.”
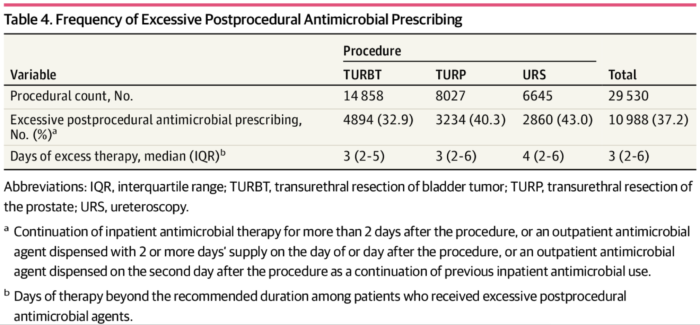
To reach those conclusions, the study team manually reviewed the medical records from January 2016 to July 2017 of 375 VHA patients who had one of three common urological procedures, all of which use endoscopic devices inserted into the urethra to examine and manipulate portions of the urinary tract. Also reviewed was administrative data from 29,530 patient records from the entire VHA system.
Results indicated that a majority, about 58%, of patients were prescribed antibiotics in a guideline-discordant manner.
Researchers reported that postprocedural antimicrobial agents were continued beyond 24 hours in 56.3% of patients and were guideline discordant in 83.9%, with a median (interquartile range) duration of 3 (3-5) days of unnecessary antimicrobial therapy.
National administrative data showed that excessive postprocedural antimicrobial agents were prescribed in 37.2% of surgical patients, with a median (interquartile range) of 3 (2-6) excess days.
“If a patient undergoing surgery is given antibiotics for more than 24 hours, he or she should ask the provider to explain why more antibiotics are necessary,” Livorsi said.
The researchers documented variation in excessive postprocedural antimicrobial use across the more than 80 VHA sites included in the national analysis. Interfacility variation in excessive postprocedural antimicrobial prescribing ranged from 14.7% to 62.3%, they reported, noting, “Such a high degree of interfacility variability may reflect a lack of guideline awareness, patient-specific factors that vary across sites and skepticism about guideline recommendations among certain prescribers. The interfacility variability may also reflect differences in the process of prescribing across sites. For example, some facilities may rely more heavily on physicians-in-training or automated protocols to prescribe antimicrobial prophylaxis, which could affect the frequency of guideline concordance.”
The VA system was chosen for the study because it is the largest integrated health care system in the United States, but Livorsi suggested the results are not unique to the VA.
Background information in the report noted that surveys have suggested that urologists vary greatly in their perceived adherence to the professional guidelines, with one previous study using a large healthcare database to assess antimicrobial appropriateness in patients who had urologic procedures from 2007 to 2012, finding that AUA guidelines were followed less than 60% of the time.
Researchers recommended a focus on the post-procedure period for reduced antibiotic prescribing.
While preprocedural screening and treatment for bacteriuria were found to be largely appropriate, both were frequently performed well before the procedure, according to the study, which noted that AUA guidelines are unclear on when to screen and treat for asymptomatic bacteriuria.
“These findings would seem to support the recommendations from the Infectious Diseases Society of America: antimicrobial treatment for asymptomatic bacteriuria should be initiated immediately before the procedure and stopped immediately after the procedure,” study authors advised.
1. Khaw C, Oberle A, Lund BC, Egge J et. Al. Assessment of Guideline Discordance With Antimicrobial Prophylaxis Best Practices for Common Urologic Procedures. JAMA Netw Open. 2018;1(8):e186248. doi:10.1001/jamanetworkopen.2018.6248
