Infection from the respiratory syncytial virus is usually mild in adults unless they are older or have co-morbidities. A new study revealed that 14.5% of hospitalized adults aged 50 years or older with RSV infection experienced acute heart failure, which was a higher prevalence than with influenza or COVID-19 infection. The solution, according to public health officials, is for older adults such as the more than one-third of VHA patients 70 or older, receive an effective vaccine against RSV.
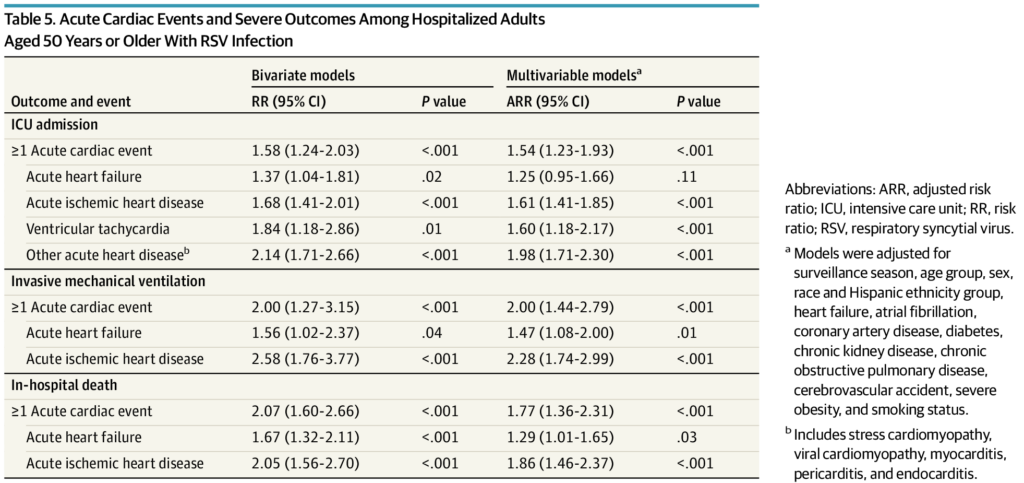
Click to Enlarge: Acute Cardiac Events and Severe Outcomes Among Hospitalized Adults Aged 50 Years or Older With RSV InfectionAbbreviations: ARR, adjusted risk ratio; ICU, intensive care unit; RR, risk ratio; RSV, respiratory syncytial virus.
a. Models were adjusted for surveillance season, age group, sex, race and Hispanic ethnicity group, heart failure, atrial fibrillation, coronary artery disease, diabetes, chronic kidney disease, chronic obstructive pulmonary disease, cerebrovascular accident, severe obesity, and smoking status.
b. Includes stress cardiomyopathy, viral cardiomyopathy, myocarditis, pericarditis, and endocarditis. Source: JAMA Network Open
ATLANTA — Immunization levels against respiratory syncytial virus (RSV) among older adults remained relatively low at around 24% as of late March. As a comparison, national coverage with influenza vaccines for all U.S. adults was 48.3% in the same time period, 2% higher than last year.
Yet, evidence is mounting that, in many ways, RSV can be as dangerous as influenza and even COVID-19 in some situations for older adults. That is especially the case in a population like the veterans treated by the VHA. In 2023, 37% of U.S. military veterans were 70 or older, and veterans were more likely to have serious comorbidities that most of the general population.
The latest study pointed out that while it is well understood that RSV can cause severe respiratory illness in older adults, not as much is known about the cardiac complications of RSV disease compared with those of influenza and SARS-CoV-2 infection.
Researchers, including participation from the Atlanta VAMC, sought to describe the prevalence and severity of acute cardiac events during hospitalizations among adults age 50 years or older with RSV infection. Their results appeared in JAMA Internal Medicine.1
The cross-sectional study analyzed surveillance data from the RSV Hospitalization Surveillance Network, which conducts detailed medical record abstraction among hospitalized patients with RSV infection detected through clinician-directed laboratory testing. The team examined cases of RSV infection in adults aged 50 years or older within 12 states over five RSV seasons—annually from 2014-2015 through 2017-2018 and 2022-2023—were examined to estimate the weighted period prevalence and 95% CIs of acute cardiac events.
The focus was on acute cardiac events, as well as severe disease outcomes, including intensive care unit (ICU) admission, receipt of invasive mechanical ventilation or in-hospital death. The authors calculated adjusted risk ratios (ARR) to compare severe outcomes among patients with and without acute cardiac events.
Included in the study were 6,248 hospitalized adults (median [IQR] age, 72.7 [63.0-82.3] years; 59.6% female; 56.4% with underlying cardiovascular disease) with laboratory-confirmed RSV infection.
Results indicated that the weighted estimated prevalence of experiencing a cardiac event was 22.4% (95% CI, 21.0%-23.7%). The weighted estimated prevalence was 15.8% (95% CI, 14.6%-17.0%) for acute heart failure, 7.5% (95% CI, 6.8%-8.3%) for acute ischemic heart disease, 1.3% (95% CI, 1.0%-1.7%) for hypertensive crisis, 1.1% (95% CI, 0.8%-1.4%) for ventricular tachycardia, and 0.6% (95% CI, 0.4%-0.8%) for cardiogenic shock.
“Adults with underlying cardiovascular disease had a greater risk of experiencing an acute cardiac event relative to those who did not (33.0% vs 8.5%; ARR, 3.51; 95% CI, 2.85-4.32),” the researchers advised. “Among all hospitalized adults with RSV infection, 18.6% required ICU admission and 4.9% died during hospitalization. Compared with patients without an acute cardiac event, those who experienced an acute cardiac event had a greater risk of ICU admission (25.8% vs. 16.5%; ARR, 1.54; 95% CI, 1.23-1.93) and in-hospital death (8.1% vs. 4.0%; ARR, 1.77; 95% CI, 1.36-2.31).”
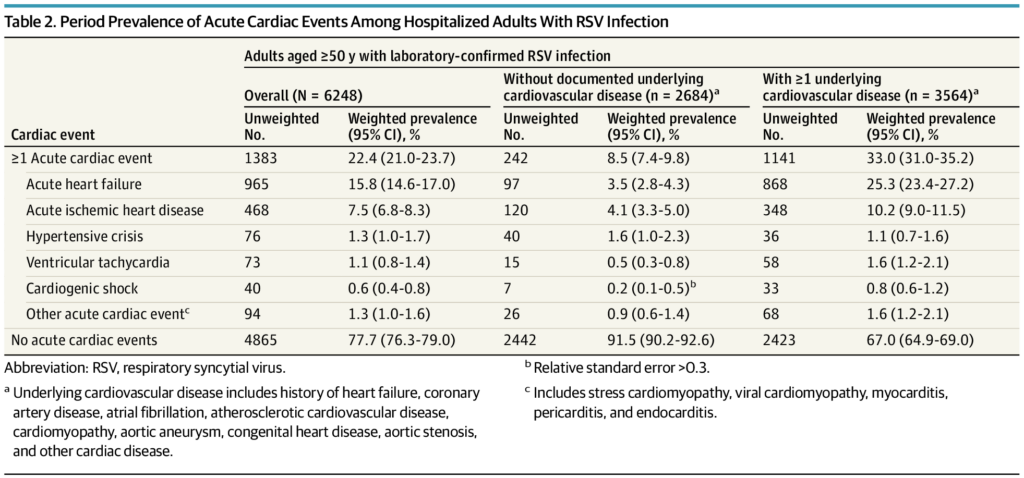
Click to Enlarge: Period Prevalence of Acute Cardiac Events Among Hospitalized Adults With RSV InfectionAbbreviation: RSV, respiratory syncytial virus.
a. Underlying cardiovascular disease includes history of heart failure, coronary artery disease, atrial fibrillation, atherosclerotic cardiovascular disease, cardiomyopathy, aortic aneurysm, congenital heart disease, aortic stenosis, and other cardiac disease.
b. Relative standard error >0.3.
c. Includes stress cardiomyopathy, viral cardiomyopathy, myocarditis, pericarditis, and endocarditis. Source: JAMA Network Open
The study team emphasized that, over five RSV seasons, “nearly one-quarter of hospitalized adults aged 50 years or older with RSV infection experienced an acute cardiac event (most frequently acute heart failure), including 1 in 12 adults (8.5%) with no documented underlying cardiovascular disease. The risk of severe outcomes was nearly twice as high in patients with acute cardiac events compared with patients who did not experience an acute cardiac event. These findings clarify the baseline epidemiology of potential cardiac complications of RSV infection prior to RSV vaccine availability.”
Background information in the article noted that RSV is a seasonal respiratory virus that usually causes mild upper respiratory tract symptoms, although it can cause severe lower respiratory tract disease in high-risk groups.
“Among adults, older age and history of chronic medical conditions, including heart failure and coronary artery disease, are risk factors for severe RSV illness requiring hospitalization,” the authors pointed out, adding that RSV has been associated with annual totals of up to 160 000 hospitalizations, 10 000 deaths, and $4.0 billion in direct healthcare costs among U.S. adults age 65 years or older.
Severity ‘Underappreciated’
“However, despite evidence of considerable RSV-associated morbidity, mortality, and health care expenditure, the potential severity of RSV infection in adults has historically been underappreciated by public health professionals and clinicians,” the researchers emphasized. “Surveillance for RSV-associated illness in adults has been hampered by infrequent clinical testing, as clinicians may choose not to test because of limited awareness of RSV as an important pathogen in adults and because an RSV diagnosis does not typically change patient management.
“Additionally, until recently, limited tools were available to prevent RSV infection, although this changed in 2023 when the first RSV vaccines for adults aged 60 years or older were approved and recommended in the U.S. via the use of shared clinical decision-making, which takes into account the risks and benefits of RSV disease and vaccination, the clinician’s knowledge and experience, and the patient’s values and preferences.”
The CDC advised that there are two RSV vaccines licensed for use in adults age 60 years and older in the United States: GSK Arexvy and Pfizer Abrysvo. The agency recommends that adults 60 years of age and older may receive a single dose of RSV vaccine using shared clinical decision-making (SCDM). This means that healthcare providers and their patients should have a conversation to determine if RSV vaccination will be beneficial.
The recommendation differs, however, from routine age-based and risk-based vaccine recommendations for which the default decision is to vaccinate everyone in a specified age group or risk group.
“Under SCDM, there is no default,” the CDC explains on its website. “Rather, the decision whether to vaccinate a patient is individually based and informed by discussions between the patient and health care provider (anyone who provides or administers vaccines, including primary care physicians, specialists, physician assistants, nurse practitioners, registered nurses, and pharmacists).”
The recent study suggested that “comprehensive data about potential cardiac complications of RSV infection, similar to what are available for hospitalizations for influenza or SARS-CoV-2 infections, could help guide clinical and public health practices, characterize the burden of RSV-associated cardiovascular disease prior to the introduction of novel vaccines, and prompt studies evaluating the prevention of acute cardiac events through RSV vaccination.”
The research focused on adults 50 years or older, because that cohort accounts for more than 90% of RSV-associated hospitalizations of adults in the United States. In addition, the study team added that their results are important “In light of emerging clinical trial data in adults aged 50 to 59 years, which could expand RSV vaccination to younger age groups. Additionally, we sought to identify risk factors for experiencing an acute cardiac event and to determine whether acute cardiac events are independently associated with increased risk of severe outcomes during hospitalization.”
Results from the study bolstered previous findings that acute heart failure, coronary events and atrial fibrillation occur frequently among adults hospitalized with acute respiratory infections, including influenza and SARS-CoV-2. “Notably, we found that 14.5% of hospitalized adults aged 50 years or older with RSV infection experienced acute heart failure,” the authors wrote. “This prevalence was higher than in similarly aged hospitalized adults with laboratory-confirmed influenza or COVID-19 infection (5.5% to 9.0% for influenza-associated hospitalizations and 4.0% to 8.5% for COVID-19–associated hospitalizations, depending on the age group) and is consistent with prior studies indicating that adults with chronic heart failure are at increased risk of severe illness from RSV infection.
“Acute ischemic heart disease occurred as often among hospitalized adults aged 50 years or older with RSV infection as among similarly aged hospitalized adults with laboratory-confirmed influenza or COVID-19 infection (4.1% to 9.0% for influenza-associated hospitalizations and 5.1% to 7.8% for COVID-associated hospitalizations, depending on the age group).”
The study advised that the pathophysiology by which respiratory viral infection could result in acute cardiac events has not been established. It posited that it might include both pathogen-specific and nonspecific mechanisms. “Hypothesized mechanisms include increased cytokine-related inflammatory responses that contribute to coronary plaque destabilization, hypercoagulability resulting in an increased risk of thromboses, demand ischemia due to physiologic and metabolic stress from acute respiratory illness, direct myocardial injury, and indirect consequences from the strain on the respiratory tract, all of which may occur with RSV infection,” according to the study.
The authors point out that both RSV vaccines approved for adults were shown to be effective in preventing symptomatic RSV lower respiratory tract disease in older adults but added that clinical trials were underpowered to estimate effectiveness against more severe disease, including disease requiring hospitalization.
“Prevention of acute cardiac events may be another important consideration for postlicensure studies of the impact of RSV vaccines, especially among older adults with risk factors for such events identified in this study,” they suggested. “Indeed, influenza vaccination has been associated with reduced risk of acute cardiovascular events in the hospital setting. With additional candidate RSV vaccines in clinical trials and potential expansion of RSV vaccination to adults aged 50 to 59 years, interest in this topic is likely to grow.
“This study demonstrates the prevaccine epidemiology of acute cardiac events among adults with RSV-associated hospitalization, which represents a substantial burden of potentially vaccine-preventable disease.”
- Woodruff RC, Melgar M, Pham H, et al. Acute Cardiac Events in Hospitalized Older Adults With Respiratory Syncytial Virus Infection. JAMA Intern Med. Published online April 15, 2024. doi:10.1001/jamainternmed.2024.0212

