Renal cell carcinoma (RCC) makes up more than 90% of malignancies of the kidneys, and the World Health Organization recently delineated 21 subtypes. Among those are molecularly defined renal carcinomas. The researchers said the more specific understanding of cancer types is expected to aid treatment.
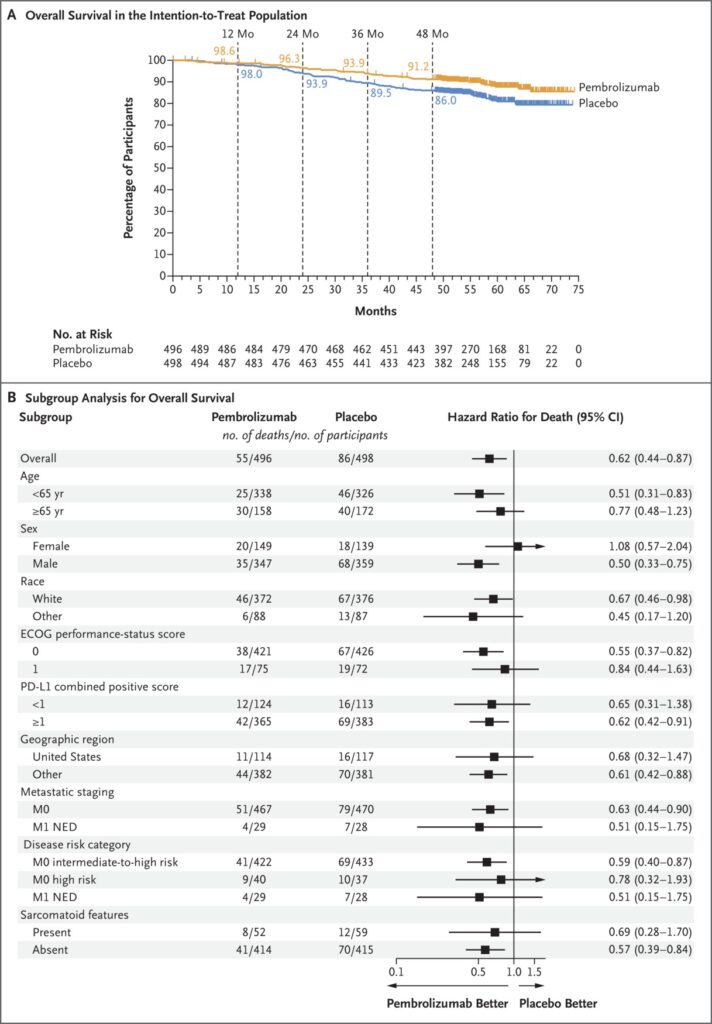
Click to Enlarge: Overall Survival (Intention-to-Treat Population). Source: The New England Journal of Medicine
RICHMOND, VA — Forty years ago, the only recognized form of kidney cancer was renal cell carcinoma (RCC). Today, RCC still accounts for more than 90% of malignancies in the kidney, but now the World Health Organization (WHO) delineates 21 subtypes, with significant differences in aggressiveness and treatment options.
Further, the latest WHO classification system of urinary and male genital tumors expands beyond the location, morphologic and immunohistochemical characterizations of previous categorizations to include an entirely new group, molecularly defined renal carcinomas.
Three new types of tumors are delineated in the classification system: elongin C (ELOC)-mutated renal cell tumors, eosinophilic solid cystic renal cell tumors and anaplastic lymphoma kinase (ALK)-rearranged renal cell tumors. In addition, the first molecularly defined type, previously known as Xp11.2 translocation RCC, received a new name, TFE3-rearranged RCC. Others in the category include TFEB-altered, fumarate hydratase-deficient, succinate dehydrogenase-deficient, and SMARCB1-deficient renal medullary carcinoma.
Researchers at the McGuire Hunter VAMC in Richmond, VA, and Virginia Commonwealth University (VCU) School of Medicine recently dove into the implications for treatment and development of RCC therapies arising from the new category in an article in Urologic Oncology.1
TFE3-rearranged RCC: While several of the molecularly defined malignancies are more indolent than clear cell RCC (ccRCC), the most common type of kidney cancer, TFE3-rearranged RCC is at least equally aggressive, particularly in older patients, such as those treated by the VA. For early-stage disease, the authors recommend radical surgical excision along with lymphadenectomy in children. For advanced disease, no standard of care has been developed, but the National Comprehensive Cancer Network (NCCN) guidelines note that this type has shown some response to combined tyrosine kinase inhibitor/immunotherapy approaches. A phase II clinical trial evaluating the use of axitinib plus nivolumab in unresectable or metastatic TFE3-rearranged RCC is in progress.
TFEB-altered RCC: TFEB-rearranged mutation is most often seen in younger patients, often in their 30s, and is typically more indolent than TFE3-rearranged RCC or ccRCC, whereas the more aggressive TFEB-amplified RCCs are found in patients of about 60 years of age. Both are included in this new category. In the absence of a recommended systemic treatment, the researchers emphasized the need for interdisciplinary consultation for treatment planning. They also noted that the vascular endothelial growth factor receptor pathway is a possible therapeutic target and that some reports indicate durable complete response to PD-L1 inhibitor therapy.
ELOC-mutated RCC: Formerly known as TCEB1-mutated RCC, ELOC-mutated RCC typically affects men aged 40 and older. Studies are mixed on the degree of aggressiveness of this subtype, and recommendations for treatment are lacking.
Fumarate hydratase (FH)-deficient RCC: Immunohistochemical analysis of FH-deficient RCCs often find complete loss of FH expression. It is notable for its rapid progression, with Steven Smith, MD, PhD, and Lance Hampton, MD, both of the Richmond VAMC and VCU and their colleagues noting that “this rare and remarkably aggressive entity is frequently metastatic at presentation, with ∼75% of cases staged as pT3 or pT4 at nephrectomy.” Guidelines recommend weighing use of erolotinib and bevacizumab or immunotherapy-based treatments for metastatic disease.
Succinate dehydrogenase (SDH)-deficient RCC: A very rare subtype, SDH-deficient RCC is often diagnosed in patients in their 30s. Fortunately, surgery is frequently curative, the authors noted.
Anaplastic lymphoma kinase (ALK)-rearranged RCC: There are two subtypes of ALK-rearranged RCC with one characterized by a fusion between vinculin and ALK and the second by rearrangements between ALK and other partners. The subtypes differ in location, histology and demographic distribution, with the VCL::ALK fusion subtype typically appearing in the renal medulla and predominant in patients of African descent who have sickle cell trait. The second subtype appears to be more aggressive, with one-third of patients exhibiting metastases at diagnosis. It also seems to disproportionately affect of East Asian descent. “Management-wise, surgical resection is indicated for local disease, though in systemic disease, treatment with ALK kinase inhibitors such as entrectinib has shown very promising results,” the researchers said.
SWI/SNF Related, Matrix Associated, Actin Dependent Regulator of Chromatin, Subfamily B, Member 1 (SMARCB1)-deficient renal medullary carcinoma: “A particularly rare and extremely aggressive cancer that almost exclusively affects patients carrying the sickle cell trait, with a predilection for males,” SMARCB1-deficient renal medullary carcinoma frequently is first diagnosed at stage IV and has a mortality rate of 95%, with median survival time of about 14 months, Smith, Hampton and colleagues noted. If resection is possible, radical nephrectomy with retroperitoneal lymph node dissection is recommended with metastatic disease treated with several combinations of conventional cytotoxic agents, although “consideration of clinical trial participation is urged given recent rapid growth of understanding of the molecular biology of these most aggressive renal tumors,” the authors added. A number of trials are in process for this tumor type.
While clear recommendations for treatment are not yet available given the recent characterization of molecularly defined RCC and their relative rarity, the new classification still provides value to clinicians and researchers.
“While molecular classification of RCC has increased diagnostic complexity and engendered need for resources in ancillary testing, review of the current and emerging management considerations of the tumors described herein supports the clinical value of their recognition and diagnosis to patients, pathologists, and urologic oncologists,” said Smith, Hampton and colleagues. “One additional advantage of this new category of tumors, bears mention as well—the conceptual separation of diagnostic categories from syndromic terms.”
- Kanakaraj J, Chang J, Hampton LJ, Smith SC. The New WHO Category of “Molecularly Defined Renal Carcinomas”: Clinical and Diagnostic Features and Management Implications. Urol Oncol. 2024 Mar 21:S1078-1439(24)00333-8. doi: 10.1016/j.urolonc.2024.02.003.

