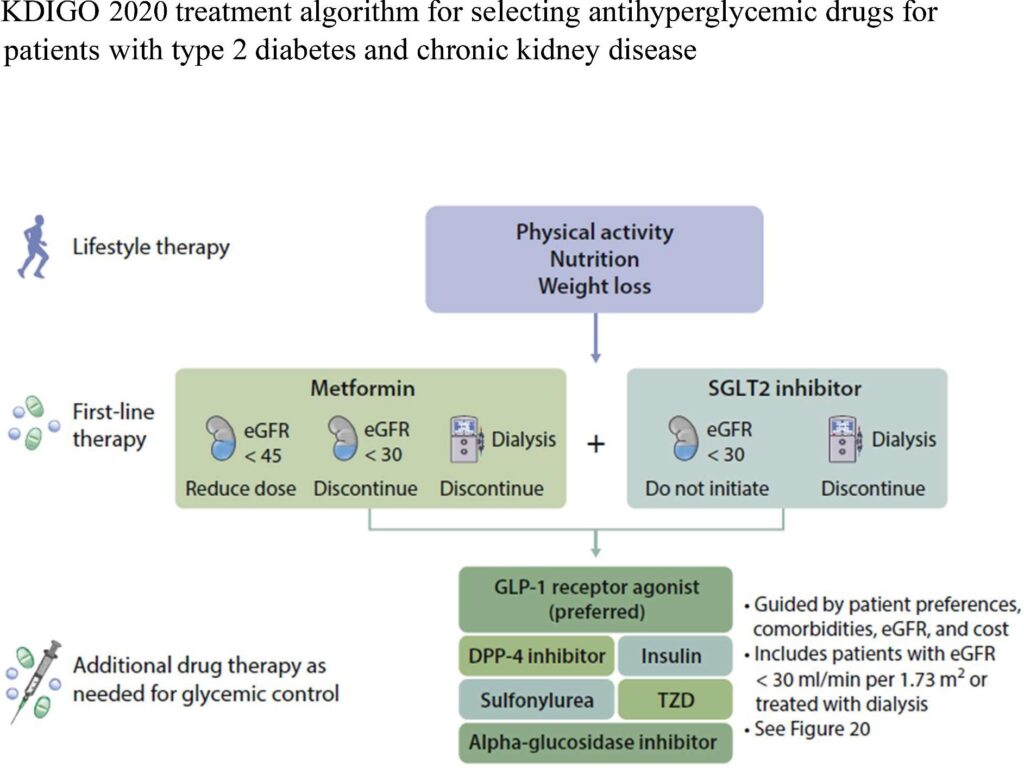
Click to Enlarge: KDIGO 2020 treatment algorithm for selecting antihyperglycemic drugs for patients with type 2 diabetes and chronic kidney disease. KDIGO, Kidney Disease: Improving Global Outcomes; eGFR, estimated glomerular filtration rate; DPP-4, dipeptidyl peptidase-4; GLP-1, glucagon-like peptide-1; SGLT2, sodium–glucose cotransporter-2; TZD, thiazolidinedione. Source: Nephrology Dialysis Transplantation
BETHESDA, MD — While news reports focus on high demand for glucagon-like peptide-1 receptor agonists (GLP-1 RA), the real story might be widespread under use of those agents and others that reduce the risk of cardiovascular disease and chronic kidney disease progression in patients with Type 2 diabetes.
A recent study from Walter Reed National Military Medical Center and the Uniformed Services University, both in Bethesda, MD, decried hesitancy to prescribe guideline-directed drug therapies, including GLP-1 RAs, that offer substantial cardiorenal benefits, improved quality of life and longevity in patients with chronic kidney disease (CKD) and Type 2 diabetes. Other treatment options include sodium-glucose cotransporter-2 inhibitors (SGLT2i) and non-steroidal mineralocorticoid receptor antagonists.
“However, despite compelling evidence from multiple clinical trials, their uptake has been slow in routine clinical practice, reminiscent of the historical evolution of angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker use,” the authors wrote in Nephrology Dialysis Transplantation.1
The VA hasn’t fared much better. Prescription rates remain low for novel therapies for Type 2 diabetes therapies that have been proven to reduce the risk of cardiovascular disease and chronic kidney disease progression. Compounding the issue is that, compared with white veterans, those of all other racial groups had significantly lower odds of prescriptions for sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA), with Hispanic patients the least likely.
A study in JAMA last year looked at prescription equitability among more than 1 million patients with Type 2 diabetes. The cross-sectional analysis used data from the VHA’s Corporate Data Warehouse. Included in the study were adult patients with type 2 diabetes and at least two primary care clinic visits from Jan. 1, 2019, to Dec. 31, 2020.
Researchers from the University of California, San Francisco and the San Francisco VA Healthcare System defined the primary outcomes as any active SGLT2i or GLP-1 RA prescription during the study period.2
The 1.2 million VHA patients, 96% men, had a mean age of 68 years. The racial/ethnic breakdown was:
- 1% American Indian or Alaska Native,
- 2% Asian, Native Hawaiian, or Other Pacific Islander,
- 7% of Hispanic or Latino,
- 20% Black or African American, and
- 71% white.
During the study period, only 10.7% and 7.7% were prescribed an SGLT2i or a GLP-1 RA, respectively. Researchers reported that prescription rates for SGLT2i and GLP-1 RA, respectively, were 11% and 8.4% among American Indian or Alaska Native patients; 11.8% and 8% among Asian, Native Hawaiian or Other Pacific Islander patients; 8.8% and 6.1% among Black or African-American patients; and 11.3% and 8.2% among white patients, respectively.
Prescription rates for SGLT2i and GLP-1 RA, respectively, were 11% and 7.1% among Hispanic or Latino patients and 10.7% and 7.8% among non-Hispanic or Latino patients.
“After accounting for patient- and system-level factors, all racial groups had significantly lower odds of SGLT2i and GLP-1 RA prescription compared with white patients. Black patients had the lowest odds of prescription compared with white patients (adjusted odds ratio, 0.72 [95% CI, 0.71-0.74] for SGLT2i and 0.64 [95% CI, 0.63-0.66] for GLP-1 RA),” the study authors pointed out. “Patients of Hispanic or Latino ethnicity had significantly lower odds of prescription (0.90 [95% CI, 0.88-0.93] for SGLT2i and 0.88 [95% CI, 0.85-0.91] for GLP-1 RA) compared with non-Hispanic or Latino patients.”
The authors called for further research to better understand why those underlying prescribing differences exist and how they affect clinical outcomes.
- Nee R, Yuan CM, Narva AS, Yan G, Norris KC. Overcoming barriers to implementing new guideline-directed therapies for chronic kidney disease. Nephrol Dial Transplant. 2023 Feb 28;38(3):532-541. doi: 10.1093/ndt/gfac283. PMID: 36264305; PMCID: PMC9976771.
- Lamprea-Montealegre JA, Madden E, Tummalapalli SL, et al. Association of Race and Ethnicity With Prescription of SGLT2 Inhibitors and GLP1 Receptor Agonists Among Patients With Type 2 Diabetes in the Veterans Health Administration System. JAMA. 2022;328(9):861–871. doi:10.1001/jama.2022.13885

