Well-timed colonoscopy appears to improve overall survival in inflammatory bowel disease patients, but many VA patients aren’t getting screened regularly. A new study supported current VA practice guidelines that recommend colonoscopy intervals from one year to three years among patients with IBD who have extensive colitis or left-sided colitis.
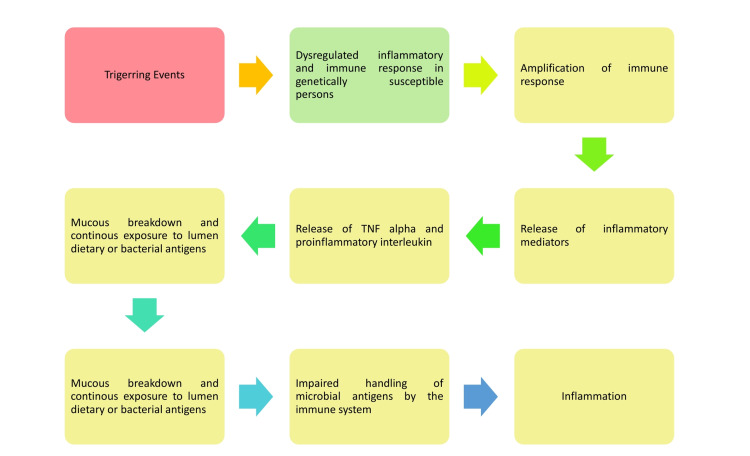
Click To Enlarge: Pathophysiology of inflammatory events in IBD
IBD: inflammatory bowel disease Source: Cureus. 2022 Feb; 14(2): e22636.
HOUSTON — Because inflammatory bowel disease (IBD) significantly increases the risk of colorectal cancer (CRC), guidelines recommend that patients with Crohn’s disease or ulcerative colitis receive colonoscopies more frequently than the every 10 years recommended for individuals over age 50 with normal risk of CRC.
But just how frequently and how much benefit there is to surveillance colonoscopy has remained murky due to the lack of randomized controlled trials—and the ethical issues with attempting one.
Finding the right interval is a matter of significance to the VA, as the agency diagnoses about 4,000 new cases of colorectal cancer each year. That makes it the third most diagnosed malignancy in the nation’s largest healthcare system.
“The VA does an extraordinary job of getting veterans screened,” Folosade May, MD, staff gastroenterologist at the West Los Angeles VAMC told U.S. Medicine previously. “While 1 in 3 Americans remains unscreened, 82% to 84% of veterans are current on their screening today.”
The American Gastroenterology Association notes that “the optimal surveillance interval has not been clearly defined. After two negative examinations (no dysplasia or cancer), further surveillance examinations should be performed every one to three years.” Other society guidelines recommend intervals between one and five years. Increased surveillance colonoscopy is not recommended for individuals with isolated ileal or rectal disease.
Frequent colonoscopies are unpleasant at best, which makes convincing patients to undergo them challenging, particularly without compelling evidence. To gain greater clarity on the best interval for veterans with IBD, researchers at the Michael E. DeBakey VAMC in Houston and the VA Ann Arbor, MI, Healthcare System, along with colleagues across the country, conducted a retrospective cohort study of 566 veterans with confirmed CRC within a cohort of 77,824 patients with IBD. The study used 15 years’ worth of data from the VHA.
Of the 566,358 had underlying ulcerative colitis, 195 had Crohn’s disease, and 13 had unclassified IBD. The average age of IBD diagnosis was 53.6 years and the mean age of CRC diagnosis was 67.5 years.
The team compared multiple intervals between last colonoscopy before CRC diagnosis, excluding any within six months of diagnosis: none, annual (six months to a year), within one to three years, and within three to five years, with the intervals set based on those recommended by various professional societies. More than five years was considered “none.” as all guidelines advise screening this population at least every five years.
Most Had No Colonoscopy
Nearly 70% of the veterans had not received a coloscopy within five years of their CRC diagnoses, while 9.7% had received one within the year, 17.7% within one to three years, and 3.1% within three to five years. Those who had no colonoscopy generally had not been diagnosed with IBD as long as veterans who were screened within one to five years, with mean duration of IBD of 12.4 years compared to 15.7 to 17.7 years, respectively.
In 337 cases, stage at diagnosis was available. Among these, coloscopy interval of less than one year reduced the risk of a late-stage disease diagnosis by 60% and screening within one to three years reduced the risk 44% compared to no colonoscopy. The researchers found no association between race/ethnicity, IBD type or extent, smoking or alcohol use, comorbidities or IBD facility volume and tumor stage.
Overall, 87% of veterans with CRC received treatment, with the percentage rising to 96% among those with early-stage disease. A multivariate analysis revealed the only significant variable in treatment for CRC was disease stage.
During the study, 70% of veterans died, with 23% of deaths related to CRC. The researchers found that “colonoscopy interval did not significantly affect CRC-related mortality compared with no colonoscopy in any of the models.” While colonoscopy within one year of CRC diagnosis had a trend toward reduced CRC-related mortality, it was not determined to be significant.
The story was different for all-cause mortality, however. On an unadjusted basis, colonoscopy less than one year prior to CRC diagnosis decreased the mortality risk 40% compared to no colonoscopy, a benefit maintained even after adjusting for lead-time bias, tumor stage, treatment, and all covariates.
Notably, screening within one year of diagnosis significantly reduced the risk of all-cause mortality compared to all other screening intervals. The no colonoscopy group and colonoscopy within one to three years groups both had 59% increase in mortality risk, while the three to five years group had more than double the risk of the within one year group.
The researchers concluded that their “findings support current practice guidelines that recommend colonoscopy intervals from one year to three years among patients with IBD who have extensive colitis or left-sided colitis.”
Furthermore, the findings may bolster clinicians’ discussions with veterans with IBD, for whom “colonoscopy is associated with significantly more embarrassment and pain” than in patients without IBD, the team noted. Painful memories can make patients less eager to schedule frequent colonoscopies. Data from this study, the researchers said, “can help patients appreciate the impact of colonoscopy on CRC outcomes.”
A recent international study published in Cureus discussed the link between chronic inflammation in UC and the link to cancer, noting “Chronic inflammation has been linked to cancer, and chronic colonic inflammation caused by IBD increases the risk of colorectal cancer (CRC)”.
The authors pointed out that, when CRC occurs in IBD patients, unlike sporadic CRC, the lesions are difficult to identify because of mucosal alterations created by inflammation.
“The total prevalence of IBD-associated CRC is increasing due to the rapidly increasing frequency of IBD,” researchers wrote. “Screening and surveillance colonoscopy in IBD patients is considered to allow for the early diagnosis of dysplasia and cancer, improving the prognosis of IBD-related CRC by giving patients proactive therapy.”
- Kim HS, Hernaez R, Sansgiry S, Waljee AK, Scott FI, Lewis JD, El-Serag HB, Hou JK. Comparative Effectiveness of Surveillance Colonoscopy Intervals on Colorectal Cancer Outcomes in a National Cohort of Patients with Inflammatory Bowel Disease. Clin Gastroenterol Hepatol. 2022 Feb 28:S1542-3565(22)00205-1. doi: 10.1016/j.cgh.2022.02.048. Epub ahead of print. PMID: 35240331.
- Rivera AP, Flores Monar GV, Islam H, Puttagunta SM, et. al. Ulcerative Colitis-Induced Colorectal Carcinoma: A Deleterious Concatenation. Cureus. 2022 Feb 26;14(2):e22636. doi: 10.7759/cureus.22636. PMID: 35371788; PMCID: PMC8959421.

