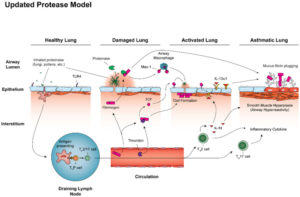
Click To Enlarge: Airway mycosis coordinates activation of the airway type 2 immune response in allergic airway disease. All persons are exposed to inhaled irritants such as pollens, but also infectious agents such as fungal spores. These exposures may trigger innate and adaptive immune responses, including Th2 and Th17 cell activation, through antigen presentation by dendritic cells, but usually without inducing disease. Lungs can become damaged, however, should fungi gain a foothold within the airway lumen and begin producing proteinases.
HOUSTON — Filamentous fungi of the Aspergillus genus and others have long been linked to the induction of type 2 immunity that underlies IgE-mediated hypersensitivity responses, but how that occurs has remained obscure.
A study led by researchers from the Michael E. DeBakey VA Center for Translational Research on Inflammatory Diseases and Baylor College of Medicine, both in Houston, sought to determine that.
Their report in the Journal of Fungi noted that the unique immune response is characterized by the production of the allergy-associated T helper cell type 2 (Th2) and Th17 cytokines interleukin 4 (IL-4), IL-13, and IL-17. Those drive IgE, eosinophilia, airway hyperresponsiveness and other manifestations of asthma, according to the authors. Type 2 immunity is promoted by proteinases secreted by filamentous fungi, but the mechanism remains unclear, they added.1
Researchers employed detailed biochemical analysis of household dust, microbiological dissection of human airway secretions and extensive modeling in mice to describe in detail how type 2 immunity evolves after exposure to fungi.
That included three key discoveries:
- Fungal proteinases drive the type 2 immune responses;
- The relationship between fungi, proteinases and type 2 immunity is explained by airway mycosis, a form of noninvasive fungal infection of the airway lumen; and
- The innate component of proteinase-driven type 2 immunity is mediated by cleavage of the clotting protein fibrinogen.
The study noted that filamentous fungi, especially Aspergillus spp., are most often acquired by inhalation of conidia and, therefore, affect the upper and lower airways. While most research in aspergillus-related disease focuses on the fungus in other organ, most aspergillus-related disease is noninvasive, with the organism remaining confined to the epithelial surface, it added.
“Superficial airway epithelial fungal infection, termed airway mycosis, is now recognized as the fundamental cause of some of the most common of human diseases, including severe asthma, chronic rhinosinusitis and their more severe brethren, allergic bronchopulmonary aspergillosis and allergic fungal rhinosinusitis,” the authors wrote. “In addition to their localized, non-invasive nature, these syndromes are distinguished from other fungal diseases by their unique immune character, marked by the presence of eosinophils, T helper type 2 (Th2) cells, Th17 cells, and other related cell types. Collectively termed type 2 immunity, a major task of immunologists and clinicians is to understand the origins and functions of type 2 immunity and the relevance of these concepts to disease expression and management.”
- Knight JM, Wu Y, Mauk K, Weatherhead J, Anvari S, Kheradmand F, Corry DB. Airway Mycosis and the Regulation of Type 2 Immunity. J Fungi (Basel). 2020 May 29;6(2):74. doi: 10.3390/jof6020074. PMID: 32485866; PMCID: PMC7344719.

