Respiratory illnesses account for a significant proportion of all noncombat diagnoses among active duty forces and veterans deployed to southwest Asia; past research estimates that more than 3% of all veterans who served in this theater had newly diagnosed asthma and a similar percentage were diagnosed with chronic obstructive pulmonary disease. How to treat those patients is even more difficult when the conditions overlap. That’s why the VA has developed recommendations for the stepwise treatment of asthma-COPD overlap syndrome.
SACRAMENTO, CA — Distinguishing asthma from chronic obstructive pulmonary disease (COPD) can pose challenges for even experienced physicians. Correctly diagnosing asthma-COPD overlap syndrome can prove harder still.
Fifteen percent to 55% of patients with a chronic obstructive airways disease have ACOS, depending on the definitions used and the population studied. These patients typically have worse outcomes than those who have either asthma or COPD alone.
For the VA, properly diagnosing and treating ACOS is particularly important.
Respiratory illnesses have accounted for a significant proportion of all noncombat diagnoses among active duty forces and veterans deployed to southwest Asia. Research from the Millennium Cohort Study found that more than 3% of all veterans who served in this theater had newly diagnosed asthma.1 A similar number of veterans have chronic obstructive pulmonary disease.
A number of professional societies and international organizations have developed their own definitions for ACOS, usually a mix of criteria including patient history, spirometry and symptoms. A more detailed and uniformly accepted definition of ACOS remains elusive, as does a standard treatment protocol.
“It is a syndrome with various phenotypes,” Timothy Albertson, MD, University of California, Davis, in Sacramento, CA, told U.S. Medicine.
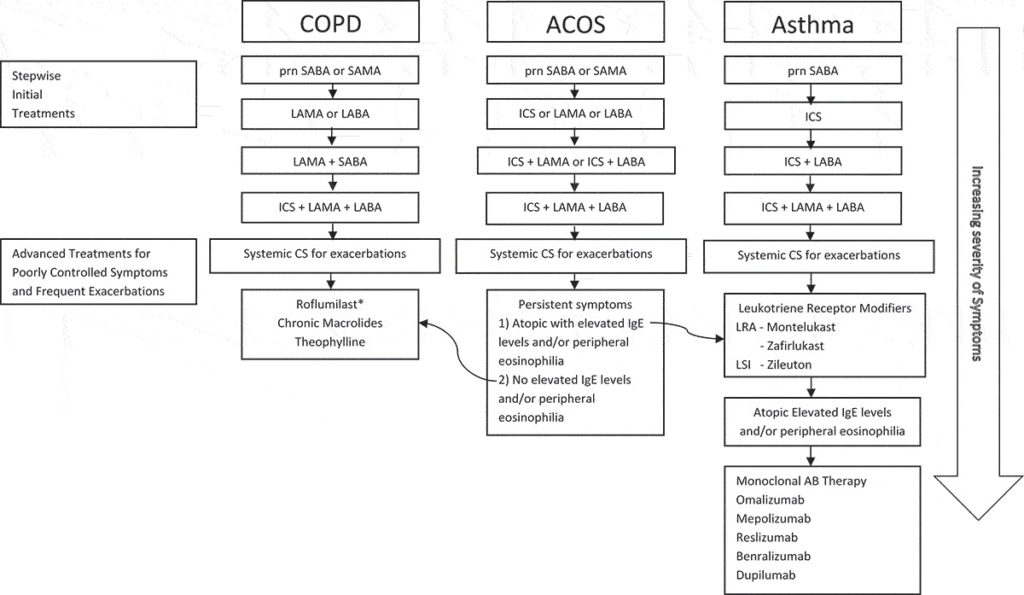
Despite the variation in presentation, Albertson and his colleagues from UC Davis and the Veterans Administration Northern California Health Care System in Sacramento recently published recommendations for the stepwise treatment of ACOS.3
They noted that, in general, asthma is characterized by allergic sensitization and T helper cell 2 lymphocytes (Th2)/eosinophil-mediated immune airway response. In contrast, COPD more typically features a T helper cell 1 (Th1)/neutrophil-mediated inflammatory process.
“Eosinophilic/Th2-mediated or Type 2 airway inflammation that also involves Type 2 innate lymphoid cells (ILC2) appears to also play an important role in many asthmatics (Type 2) and in a subgroup of COPD patients that also have asthma/atopic features,” the authors said. ACOS patients often have this type of inflammation.