Some Personnel Deployed with HbA1c of 9% or Higher
While, in general, the U.S. military will not accept recruits diagnosed with diabetes, that is especially the case with patients who use insulin, which is seen as an automatic disqualification. The situation is different, however, in military personnel already serving. While most of those retained after diagnosis have well-controlled blood sugar, about a third have hemoglobin A1c measures greater than 7%. That’s why the ability to closely monitor those servicemembers with tools such as continuous glucose monitoring is increasingly important.
Mil Med, Volume 185, Issue 3-4, March-April 2020, Pages 486–492, https://doi.org/10.1093/milmed/usz311
FORT SAM HOUSTON, TX — In most cases, the U.S. military will not accept recruits with pre-diabetes, Type 1, Type 1.5 or Type 2 diabetes. That is especially the case with patients who use insulin, which is seen as an automatic disqualification.
The situation is different, however, in those already serving. Military personnel who have well-controlled diabetes and a hemoglobin A1c below 7% often are allowed to continue, although their roles might be changed to avoid deployment.
A study in Military Medicine pointed out that U.S. military servicemembers have diabetes mellitus at a rate of 2-3%. And, despite having a chronic medical condition, they have deployed to environments with limited medical support, according to the report.
San Antonio Military Medical Center-led researchers noted the scarcity of data describing how military personnel fare in those settings, explaining why they conducted a retrospective study analyzing the changes in glycated hemoglobin (HbA1c) and body mass index (BMI) before and after deployment.
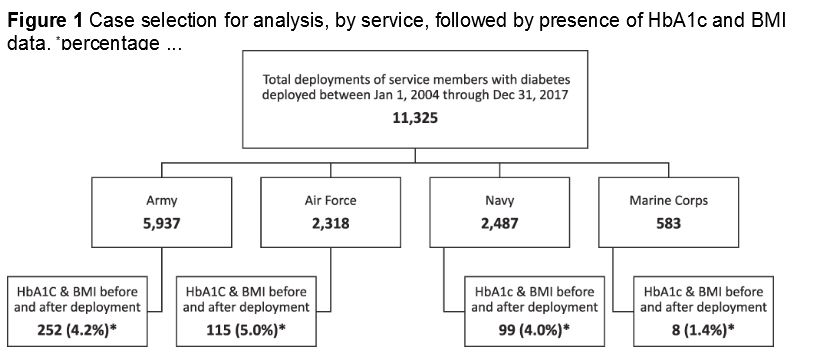
The study in Military Medicine found that servicemembers with diabetes completed 11,325 deployments of greater than 90 days from 2005 to 2017. Looking at the 474 who had both HbA1c and BMI measurements within 90 days prior to departure and within 90 days of return, the researchers came to these conclusions:
-
Most (84.2%) required diabetes medications: metformin in 67.3%, sulfonylureas in 19.0%, dipeptidyl peptidase-4 inhibitors in 13.9% and insulin in 5.5%.
-
Most deployed with an HbA1c under 7.0% (67.1%), with a mean predeployment HbA1c of 6.8%. Yet, 20% deployed with an HbA1c between 7.0 and 7.9%, 7.2% deployed with an HbA1c between 8.0 and 8.9%, and 5.7% deployed with an HbA1c of 9.0% or higher.
-
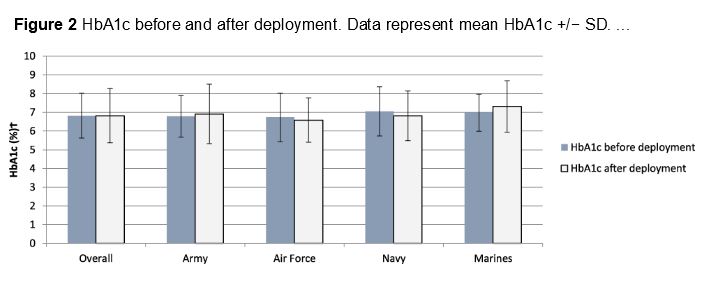
No significant change in HbA1c before or after deployment was documented.
Researchers pointed out, however, that those with predeployment HbA1c of less than 7.0% experienced a rise in HbA1c from 6.2 to 6.5%, and that those with predeployment HbA1c values of 7.0% and greater experienced an average decline from 8.0 to 7.5%.
Duration of deployment appeared to have an effect: Those who deployed between 91 and 135 days had a decline in HbA1c from 7.1 to 6.7%, although no significant changes were demonstrated in those with longer deployment durations. At the same time, BMI declined from 29.6 to 29.3 kg/m2 (P <0.001), with other significant changes seen among those in the Army and Navy and deployment durations up to 315 days.
Mil Med, Volume 185, Issue 3-4, March-April 2020, Pages 486–492, https://doi.org/10.1093/milmed/usz311
“Most SMs had an HbA1c <7.0%, suggesting that military providers appropriately selected well-managed SMs for deployment,” the authors concluded. “HbA1c did not seem to deteriorate during deployment, but they also did not improve despite a reduction in BMI.”
The study team added, “Concerning trends included the deployment of some SMs with much higher HbA1c, utilization of medications with adverse safety profiles, and the lack of HbA1c and BMI evaluation proximal to deployment departures and returns. However, for SMs meeting adequate glycemic targets, we demonstrated that HbA1c remained stable, supporting the notion that some SMs may safely deploy with diabetes. Improvement in BMI may compensate for factors promoting hyperglycemia in a deployed setting, such as changes in diet and medication availability. Future research should analyze in a prospective fashion, where a more complete array of diabetes and readiness-related measures to comprehensively evaluate the safety of deploying SMs with diabetes.”
Background information in the article pointed out that continuation of military service is possible among active duty servicemembers when they develop chronic medical conditions, such as diabetes mellitus, although multiple factors affect this decision, including occupation and severity of disease.
Duty Restrictions
“Although most military providers are aware that duty restrictions and retainability standards apply for any SM with a chronic medical condition, it is not as ubiquitously known that some have not only been retained in active duty but have also deployed,” the researchers wrote. They explained that a waiver enabling deployment is permissible as outlined by the DoD, stating that servicemembers with diabetes can participate in “contingency deployments.” That is defined as a deployment that is limited to outside the continental United States, more than 30 days in duration and in a location with medical support from only temporary military medical treatment facilities.
The guidance requires a minimum of a medical record review by a trained DoD healthcare provider to determine whether a servicemember with a chronic medical condition can deploy based on the severity and stability of the condition, as well as the environment and other anticipated requirements in deployment, according to the authors, who added, “It is logical that diabetes is specifically identified in the DoD [issuances]I as a high-risk condition since both disease decompensation and certain diabetes medications can cause incapacitation.”

