Click to Enlarge: Efficacy of a Pain Self-Management Intervention Tailored to People With HIV Source: JAMA Network Open
BOSTON — For almost three decades, antiretroviral therapy (ART) has enabled people with HIV to have nearly normal life expectancies. But as many as 85% of them experience chronic pain, due in part to common medical comorbidities and the side effects of life-saving treatments.
Addressing chronic pain is especially important in this population, given the high rates of mental health and substance-use comorbidities, making prescribing opioid pain medication risky, said authors of a new study showing the efficacy of an innovative, intensive pain self-management called Skills to Manage Pain (STOMP) for HIV patients.
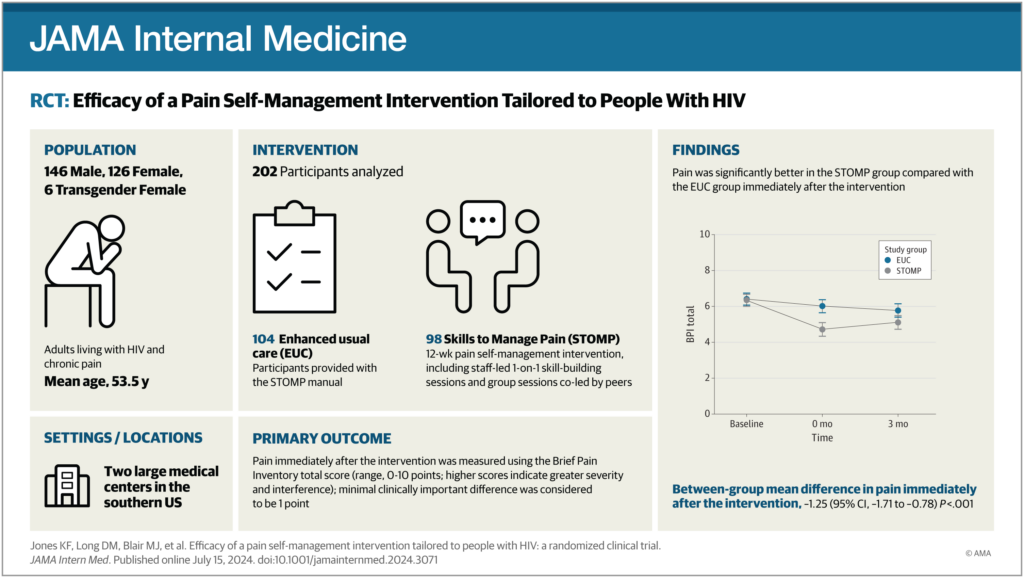
In the new study, published in JAMA Internal Medicine, STOMP was compared to usual care in 278 patients from HIV clinics at the University of Alabama at Birmingham and University of North Carolina-Chapel Hill. Participants were HIV-positive and reported at least moderate pain lasting for at least three months. Most reported multisite pain, and nearly one-quarter engaged in long-term opioid use for pain control.1
The patients were divided equally among two groups. Participants in the STOMP group received an initial one-on-one pain education session and then were asked to choose among 5 of 8 remaining sessions based on topics most interesting to them. These topics were physical activity, weight loss, relaxation, sleep, building self-worth, talking with friends and family about pain and taking opioids.
The group sessions were co-led by peer and staff interventionists. Staff interventionists were social workers and health educators trained to deliver the STOMP intervention. Peers were people with HIV with chronic pain with good communication and pain self-management skills who shared tips and strategies from one-on-one sessions and prior life experience.
The enhanced usual-care group received a copy and brief overview of the STOMP manual. Both groups continued to receive their routine care.
Before and after STOMP, the participants completed surveys on pain, pain self-efficacy and coping, the researchers reported. The main measure was the Brief Pain Inventory, which assesses pain severity and pain-related functional interference on a 0-10 scale, with higher scores indicating more pain or interference.
Right after the intervention (three months post-enrollment), participants in both groups reported a decrease in pain, although those in the STOMP group saw greater improvements—with a difference of 1.25 points on the Brief Pain Inventory, the researchers reported. “There were also immediate improvements in secondary measures, including pain self-efficacy, catastrophic thinking about pain, and depressive symptoms,” they wrote. “At three months, improvements were present but less pronounced.”
“While there’s evidence that pain self-management and peer support are crucial for dealing with chronic pain, such interventions are hard to access, because they need psychologists or other specialized clinicians and aren’t usually tailored to specific high-need groups,” said first author Katie Fitzgerald Jones, PhD, a nurse scientist and palliative and addiction nurse VA Boston Healthcare System.
“STOMP is one of the first effective pain self-management interventions specifically for people with HIV,” she told U.S. Medicine. “While the VA has been a pioneer in using peers for pain self-management, our results suggest STOMP might be more effective due to the rigorous training, the combination of peer support with one-on-one sessions and compensating peers for their time.”
Jones said STOMP is easily scalable, because the pain self-management education is delivered by clinicians “like social workers and health educators already working in HIV clinics.” For that reason, she thinks there’s potential in the future to roll out STOMP nationwide.
Further, the researchers stated the STOMP intervention also has the potential to be tailored to other highly affected groups, including cancer survivors, older adults or veterans who frequently experience multisite pain.
“Many of the investigators and I are practicing clinicians who witness the suffering associated with chronic pain, and it is incredibly satisfying to have developed and tested an intervention with such promise for improving quality of life and pain management,” she said.
“The Veterans Health Administration is a leader in promoting personalized, whole-person pain care,” Jones continued. “We’re fortunate to have pain self-management tools and peer support available through the Whole Health Systems. Clinicians should leverage these resources to help veterans live better with chronic pain.”
- Kones, K. F., Long, D. M., Bair, M. J., Agil, D., et al. (2024). Efficacy of a Pain Self-Management Intervention Tailored to People With HIV: A Randomized Clinical Trial. JAMA internal medicine, e243071. Advance online publication. https://doi.org/10.1001/jamainternmed.2024.3071
