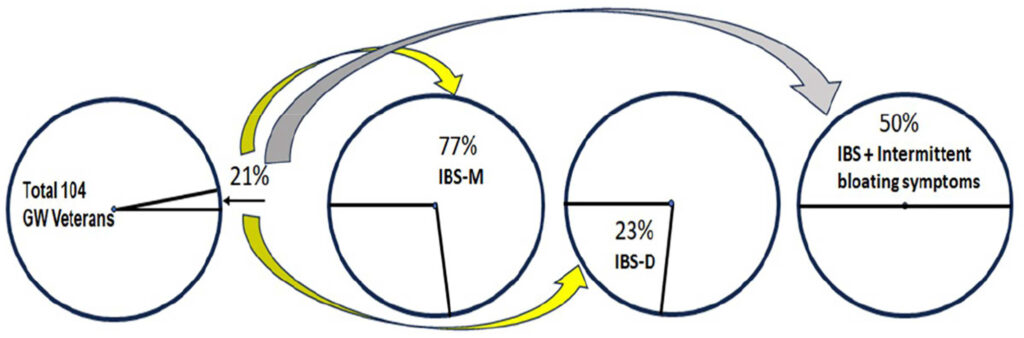
Click to Enlarge: IBS Phenotype Subset Expression in Gulf War Veterans.
Source: International Journal of Gastroenterology
MEMPHIS, TN — Deployed Gulf War veterans frequently developed several gastrointestinal symptoms, including irritable bowel syndrome, dyspepsia, diarrhea, bloating and constipation, and those often persisted long after returning home, according to a new study.
The study published in the International Journal of Gastroenterology determined the phenotypic expression, or observable traits, of gastrointestinal symptom complexes in previously healthy veterans who had been stationed in the Persian Gulf. Study authors affiliated with the VAMC in Memphis, TN, reported that theirs is the first study to classify gastrointestinal symptoms in this population.1
From Aug. 2, 1990, to July 31, 1991, an estimated 694,550 United States servicemembers were stationed in the Persian Gulf. Following their deployment, many of these veterans developed Gulf War Syndrome and chronic gastrointestinal symptoms, with more than 25% returning home with chronic gastrointestinal symptoms, the authors pointed out.
Due to the gastrointestinal symptoms, the VA Environmental Epidemiology Service reported that “evaluation, treatment and indirect costs, such as lost work, have cost more than $900 million, and these costs continue to grow. There are also concerns that many veterans currently stationed in the Persian Gulf are at increased risk for developing chronic gastrointestinal disorders,” according to the study.
The researchers evaluated the bowel habits and gastrointestinal symptoms of 104 veterans (88 males and 16 females) who were previously deployed to the Persian Gulf for a median of 16 months during the years 1990 to 1991. The veterans, who developed persistent gastrointestinal symptoms during their tour that hadn’t yet resolved, received care in VA outpatient clinics. None of the veterans had reported gastrointestinal symptoms before deployment.
For the study, a workup was completed at the Cincinnati, OH, VAMC to find identifiable causes of the veterans’ symptoms, and all participants were asked to complete a modified version of the Bowel Disease Questionnaire symptom survey.
“The study identified several gastrointestinal symptoms among previously healthy veterans who had been deployed to the Persian Gulf,” QiQi Zhou, MD, PhD., a coauthor of the study at Memphis VAMC, told U.S. Medicine. “The most common symptoms observed were diarrhea (reported by 48% of veterans), irritable bowel syndrome (21%) and dyspepsia (16%). Additionally, 11% of the veterans reported bloating, and 4% experienced constipation. These symptoms were not present before deployment and developed during or shortly after their time in the Persian Gulf. While not directly causal, this does suggest a strong association with these veterans’ military service. These findings highlight the importance of recognizing and addressing these symptoms as a potential consequence of deployment.”
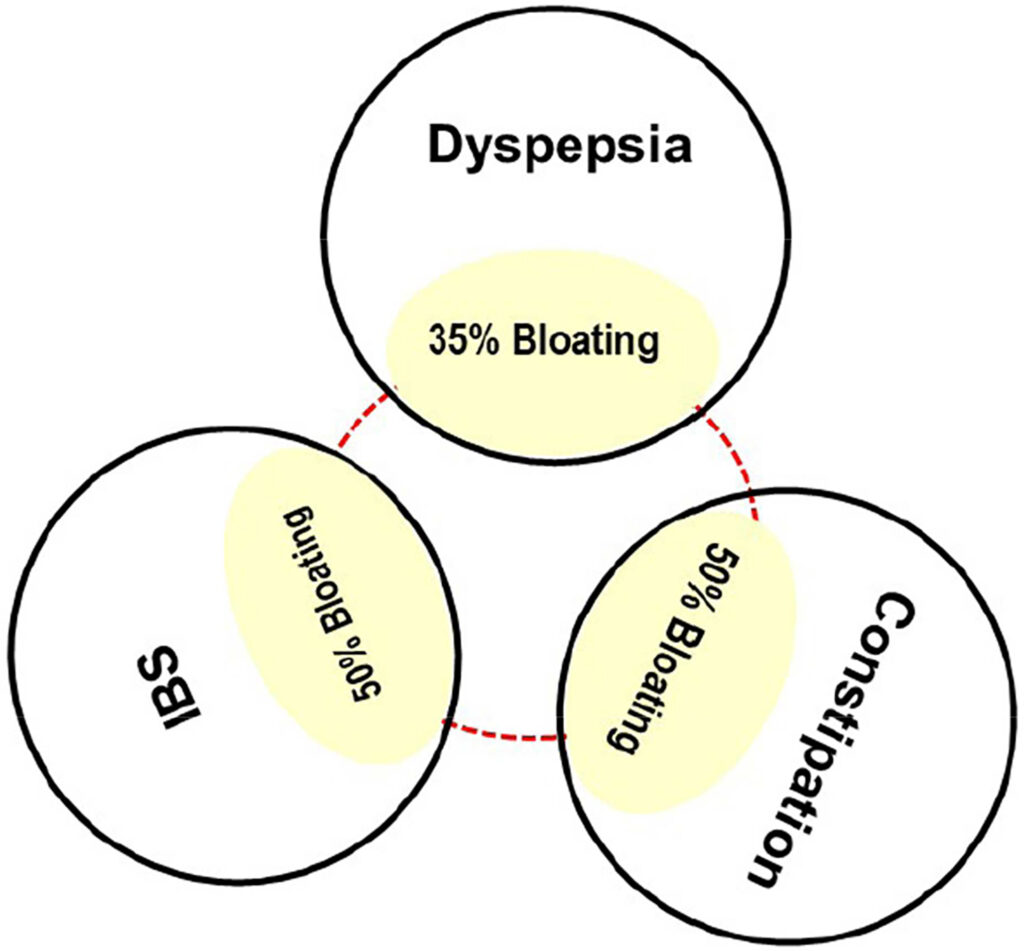
Click to Enlarge: Overlap of bloating in veterans with irritable bowel syndrome, dyspepsia, and constipation.
Source: International Journal of Gastroenterology
The results suggested that “development of irritable bowel syndrome, dyspepsia, diarrhea, bloating and constipation is frequently seen in deployed Gulf War veterans and the gastrointestinal symptoms commonly persist upon returning home. The pathophysiological mechanisms underlying the gastrointestinal symptoms in these veterans are unclear but cause significant morbidity.”
The key takeaway of the research was the “prevalence and persistence of gastrointestinal symptoms in veterans who have been deployed to the Persian Gulf,” she explained.
“Given that symptoms such as diarrhea, irritable bowel syndrome and dyspepsia were common and often persisted long after returning from deployment, it is crucial that healthcare providers routinely screen for these conditions,” Zhou suggested. “Early detection and management of these symptoms can significantly improve the quality of life for these veterans and may prevent the progression of chronic gastrointestinal disorders. Furthermore, the study underscores the importance of considering military service history when evaluating gastrointestinal complaints in veterans.”
It is recommended that healthcare professionals treating veterans who have been deployed to the Persian Gulf “incorporate routine screening for gastrointestinal symptoms as part of their standard care. Symptoms such as diarrhea, irritable bowel syndrome, dyspepsia, bloating and constipation are common and can significantly impact a veteran’s health and well-being if left untreated,” according to Zhou.
“For future service members who may be deployed to the Persian Gulf, pre-deployment assessments should include a thorough evaluation of gastrointestinal health. This proactive approach can help identify and manage any pre-existing conditions that may be exacerbated by deployment, thereby reducing the risk of chronic gastrointestinal symptoms during and after their service,” she pointed out.
The authors were motivated to study chronic gastrointestinal symptoms in Gulf War veterans because of a “longstanding recognition that military personnel frequently develop gastrointestinal complaints during and after deployment to conflict zones. Historically, such complaints have been documented among veterans from various military conflicts, making it an area of concern,” Zhou advised.
“Given the unique environmental exposures and stressors experienced by Gulf War veterans, there was a need to better understand the specific gastrointestinal symptoms they face,” she said. “This study aimed to fill a gap in knowledge, particularly in understanding the long-term gastrointestinal health of these veterans, and providing insights into how these symptoms could be managed.”
The authors noted these “novel findings are important for currently deployed veterans who are serving in the Middle East and are at a high risk of developing gastrointestinal disorders. The study’s conclusions may lead to earlier diagnosis of gastrointestinal symptom complexes for veterans who suffer from chronic gastrointestinal disorders upon returning from deployment from the Persian Gulf.”
In this study, veterans with a history of pancreatitis, inflammatory bowel disease, gastrointestinal surgery and liver disease, as well as individuals who were on a medicine that affected bowel symptoms and function, were excluded from the analysis. All participants had documented chronic gastrointestinal symptoms that they developed within two to six months after deployment and persisted upon returning home from the Persian Gulf. They previously had both upper colonoscopy and endoscopy with biopsies. A capsule endoscopy was also performed, and bacterial overgrowth was excluded with the lactulose breath test. A serum tissue transglutaminase was performed to exclude celiac sprue, and all veterans had negative stool studies including Giardia antigen along with normal hematologic and biochemical studies, according to the study.
The study’s results “support other studies on travelers who develop gastrointestinal disorders after traveling abroad, and its findings may also apply to veterans returning from other deployment assignments. Future studies of veterans from other military conflicts are needed,” the authors pointed out.
A limitation of the study is that it “focuses on Gulf War veterans enrolled in the Gulf War Registry at the VAMC in Cincinnati, OH, and it’s unclear if these findings apply to Gulf War veterans at other VAMCs. In addition, the use of patient records describing veterans who sought care may be biased and may report a higher prevalence of disorders. Lastly, a high prevalence of bowel disorders after Gulf War deployment could be attributed to increased healthcare utilization and higher reporting by the veterans after returning from deployment to the Persian Gulf,” the study authors explained.
- Verne ZT, Fields JZ, Verne GN, Zhang BB, Thacker AL, Zhou Q. Onset of Irritable Bowel Syndrome, Dyspepsia, Diarrhea, Bloating, and Constipation in Deployed Gulf War Veterans. Int J Gasteroenterol (N Y). 2024 Jun;8(1):5-10. doi: 10.11648/ijg.20240801.12. Epub 2024 Feb 5. PMID: 38487339; PMCID: PMC10935595.
