Black Patients Have Equitable Survival to Whites in VHA, MHS
Lung cancer patients, most of whom have non-small cell lung cancer (NSCLC), appeared to have fared better if treated within the VA or DoD healthcare systems. Not only are overall survival rates improving, but those universal healthcare providers provided much more equitable care so that, for example, Black veterans and servicemembers do as well or better than white ones.
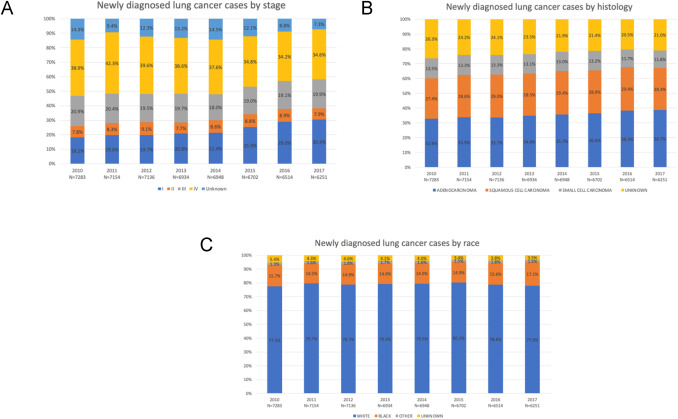
Click to Enlarge: Trends in baseline distributions at diagnosis for (A) stage, (B) histology, and (C) race. Source: Clinical Lung Cancer
LOS ANGELES — Survival rates are rising for veterans diagnosed with lung cancer within the VHA and, unlike in the general population, Black veterans are benefiting as much or more than white ones.
Researchers credited the VA’s equal access healthcare system as well an increase in the percentage of patients diagnosed at earlier stages, improved diagnostic technologies and advancements in medical, surgical and radiation therapies.
Using data from the VA Central Cancer Registry, the study team identified 54,922 veterans with lung cancer diagnosed from 2010-2017. Most of the veterans, 64.2%, had non-small cell lung cancer (NSCLC), with other histologies, including small cell lung cancer (SCLC) (12.9%) and “other” (22.9%).
“The proportion with stage I increased from 18.1% to 30.4%, while stage IV decreased from 38.9% to 34.6% (both p<0.001),” wrote the VA Greater Los Angeles Healthcare System-led researchers. “The 3-year overall survival (OS) improved for stage I (58.6% to 68.4%, p<0.001), stage II (35.5% to 48.4%, p<0.001), stage III (18.7% to 29.4%, p<0.001), and stage IV (3.4% to 7.8%, p<0.001). For NSCLC, the median OS increased from 12 to 21 months (p<0.001), and 3-year OS increased from 24.1% to 38.3% (p<0.001). For SCLC, the median OS remained unchanged (8 to 9 months, p=0.10), while the 3-year OS increased from 9.1% to 12.3% (p=0.014).”1
The study also included researchers from the VA Palo Alto, CA Healthcare System; the Atlanta VA Healthcare System; the Tennessee Valley Healthcare System in Nashville, the Durham, NC, VA Healthcare System and the VA Portland, OR, Healthcare System, as well as related academic institutions.
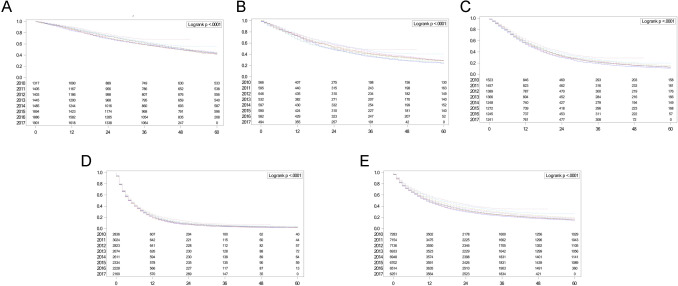
Click to Enlage: Overall survival rates for combined NSCLC and SCLC analyzed by the Kaplan-Meier method, stratified by year of diagnosis: (A) stage I, (B) stage II, (C) stage III, (D) stage IV, and (E) stage I-IV. NSCLC, non–small-cell lung cancer; SCLC, small cell lung cancer. Source: Clinical Lung Cancer
The authors pointed out that, compared to white veterans, Black veterans with NSCLC had similar OS (p=0.81), and those with SCLC had higher OS (p=0.003). “The observed racial equity in outcomes within a geographically and socioeconomically diverse population warrants further investigation to better understand and replicate this achievement in other healthcare systems,” they added. The VHA is the largest integrated healthcare system in the US and serves approximately 9 million enrollees.
The MHS, which serves approximately 9.6 million beneficiaries through TRICARE, also has reported that its patient population—active-duty servicemembers, National Guard/Reserve members, military retirees and their families—fares better than those receiving civilian care when diagnosed with lung cancer.3
Background information recounted how a New England Journal of Medicine (NEJM) report in 2020 showed improving survival rates for lung cancer patients in the United States. That study identified increasing 2-year survival rates for men (26%-35%) and women (35%-44%) diagnosed between 2001 and 2014. On the other hand, the rates of lung cancer survival increase were found to accelerate between 2013 and 2016, however. Unlike in the VHA, “while these increases were observed across different racial and ethnic groups, survival rates remained inferior throughout the study period for non-Hispanic Black men and women demonstrating the persistence of lung cancer racial disparities in the U.S.,” the authors wrote.2
That is in contrast to the findings at the VA, where, according to the more recent study, “Survival rates for veterans with lung cancer who received healthcare through the VHA increased significantly during the study period. This observation was made across all stages and histological subtypes and was coincident with the identification of a 68% relative increase in stage I at diagnosis and an 11% relative decrease in stage IV diagnosis. Further, compared to white Veterans, we observed Black Veterans with NSCLC and SCLC had better or similar survival rates, respectively”
Authors of the NEJM report from the National Cancer Institute, Harvard Medical School and the University of Michigan credited the decreases to the then-recent introduction of recommendations for routine testing of molecular alterations in epidermal growth factor receptor and anaplastic lymphoma kinase, as well as commercial use of related FDA-approved targeted therapies.
The VA authors agreed with that assessment and suggested even more contributors, such as:
- increasing utilization of low-dose chest computed tomography (LDCT) scans for early detection,
- advances in biopsy techniques to increase the likelihood of obtaining a positive biopsy and correctly staging patients at the time of initial diagnosis (e.g., endobronchial ultrasound and robotic bronchoscopy guided systems),
- incorporation of nurse navigators to improve the timeliness of care,
- technological advances improving the safety of lung cancer surgery and radiation therapy delivery systems (e.g., minimally invasive surgery and image guided radiation therapy),
- access to newly FDA-approved targeted therapies and immunotherapies,
- better integration of palliative care for patients with metastatic lung cancer which has been shown to not only prolong survival, but also improve the quality of life for people at the end of their lung cancer journey, and
- decreased wait times for healthcare within VHA since passage of the 2014 Veterans Choice Program.
“Given the complex coordination of healthcare required to successfully work up and manage patients with newly diagnosed lung cancer, further research into the relative contributions of each of these diagnostic and therapeutic factors is necessary to replicate the VHA’s success in other healthcare systems,” they added.
The researchers also noted that the achievement of better or similar survival rates in Black versus white veterans with lung cancer existed in both the VHA and MHS healthcare systems. “Collectively, these findings align with the US Military and VHA’s long-standing culture of ensuring healthcare equity which dates back to Executive Order 9881, written by President Harry S. Truman, which was declared in 1948: ‘There shall be equality of treatment and opportunity for all persons in the armed services without regard to race, color, religion or national origin.’”
Universal Healthcare Advantages
A study last year from the Murtha Cancer Center Research Program, the Uniformed Services University of the Health Sciences and the Henry M. Jackson Foundation for the Advancement of Military Medicine Inc., all in Bethesda, MD, found that the survival advantage of NSCLC patients receiving care from a universal healthcare system compared to patients from the general population was not restricted to the uninsured or those on Medicaid as expected, “but was present cross all insurance types, including patients with private insurance. Our findings highlight the survival benefits of universal health care system to lung cancer patients.”3
For the study published in Cancer Causes & Control, the researchers divided the patients from the U.S. general population by insurance status/type and compared them to the MHS patients in survival. The MHS patients were identified from the DoD’s Automated Central Tumor Registry (ACTUR). Patients from the U.S. general population were identified from the Surveillance, Epidemiology and End Results (SEER) program.3
Results indicated that, compared to ACTUR patients with NSCLC, SEER patients showed significant worse survival. The adjusted hazard ratios (HRs) were 1.08 [95% Confidence Interval (CI) = 1.03-1.13], 1.22 (95% CI = 1.16-1.28), 1.40 (95% CI = 1.33-1.47), 1.50 (95% CI = 1.41-1.59), for insured, insured/no specifics, Medicaid, and uninsured patients, respectively. “The pattern was consistently observed in subgroup analysis by race, gender, age, or tumor stage. Results were similar for small cell lung cancer (SCLC), although they were only borderline significant in some subgroups,” the study team advised.
In another study finding that cancer patients treated within the MHS generally receive their diagnoses earlier than members of the general U.S. population covered by employee-provided insurance, Medicaid or without insurance, the largest difference was noted for lung cancer, according to the researchers from Walter Reed National Military Medical Center, the Uniformed Services University of the Health Sciences, the Henry M. Jackson Foundation for the Advancement of Military Medicine Inc. and the Uniformed Services University of the Health Sciences, all in Bethesda, MD. “This difference was largest compared to the uninsured and Medicaid groups, while it was minimal for the SEER-insured groups.”
A key difference, according to the Cancer Medicine study, is that individuals, retirees and their families have free care or minimal out-of-pocket costs in the military health system (MHS). It noted that out-of-pocket costs in the United States general population can vary substantially.4
Still, lung cancer is considered very dangerous, especially among veterans and military servicemembers.
The congressionally-directed Lung Cancer Research Program (LCRP) pointed out, “Lung cancer risk for our military is significant, with 24% to as high as 38% of servicemembers smoking compared to 14% of civilians.”
The group also advised that deployments also worsen smoking rates by about 50%. Among military veterans, it explained that lung cancer is a leading cause of cancer-related deaths, with about 15 veterans dying of lung cancer each day.
“An estimated 900,000 veterans remain at risk due to age, smoking, and other environmental exposures during and after military service,” the LCRP added. “Despite improved screening methods for lung cancer and advances in treatment, the 5-year survival rate remains low at 28% for non-small cell lung cancer and only 7% for small cell lung cancer.”
- Moghanaki D, Taylor J, Bryant AK, Vitzthum LK, et. Al.. Lung Cancer Survival Trends in the Veterans Health Administration. Clin Lung Cancer. 2024 Mar 2:S1525-7304(24)00035-4. doi: 10.1016/j.cllc.2024.02.009. Epub ahead of print. PMID: 38553325.
- Howlader N, Forjaz G, Mooradian MJ, Meza R, Kong CY, Cronin KA, Mariotto AB, Lowy DR, Feuer EJ. The Effect of Advances in Lung-Cancer Treatment on Population Mortality. N Engl J Med. 2020 Aug 13;383(7):640-649. doi: 10.1056/NEJMoa1916623. PMID: 32786189; PMCID: PMC8577315.
- Lin J, Shriver CD, Zhu K. Survival among lung cancer patients: comparison of the U.S. military health system and the surveillance, epidemiology, and end results (SEER) program by health insurance status. Cancer Causes Control. 2024 Jan;35(1):21-31. doi: 10.1007/s10552-023-01765-0. Epub 2023 Aug 2. PMID: 37532916.
- Flanary JT, Lin J, Shriver CD, Zhu K. Cancer stage at diagnosis: Comparison of insurance status in SEER to the Department of Defense Cancer Registry. Cancer Med. 2023 Oct 30. doi: 10.1002/cam4.6655. Epub ahead of print. PMID: 37902129.
