Frailty in cancer patients often has been viewed as a measure of treatment tolerability, including in treatment for multiple myeloma, where there is a concern that therapy is likely to be more toxic in patients with higher levels of frailty. A new VA study found, however, that frail veterans had better survival when treated with more-intensivetherapy, although it is not clear that even greater intensity would be of benefit.
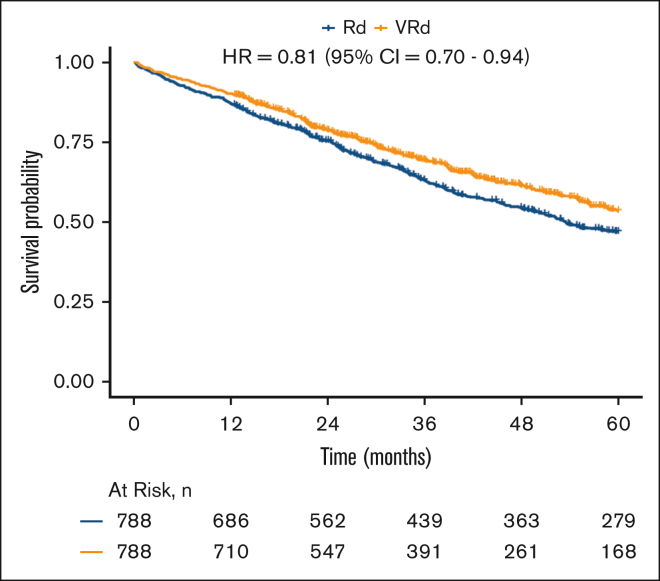
Click to Enlarge: Survival of VRd vs. Rd in combined overall population. Kaplan-Meier analyses of patients with newly diagnosed MM, evaluating differences in survival between those initially treated with VRd (orange) and those initially treated with Rd (blue), after matching based on stage and PS within each frailty category and combining these for the overall population. Source: Blood Advances
BOSTON — For frail patients with multiple myeloma, receiving more intensive therapy, triplet bortezomib-lenalidomide-dexamethasone (VRd) rather than doublet lenalidomide-dexamethasone (Rd), is a more-effective treatment, according to a recent study of patients treated in VA facilities.
The study published in Blood Advances investigated whether more-intensive therapy could be a more effective treatment for frail patients with multiple myeloma.1
The authors are affiliated with VA Boston Healthcare System and Michael E. DeBakey VAMC in Houston.
Multiple myeloma is the second-most-common blood cancer, with more than 30,000 new cases diagnosed each year. In military veterans, myeloma has been linked to Agent Orange exposure, which is relevant to the aging Vietnam-era population, who make up the growing majority of veterans treated with cancer in the VA, Clark DuMontier, MD, a researcher at VA Boston Healthcare System, told U.S. Medicine.
Based on the VA Cancer Registry, there are, on average, 800 new cases of multiple myeloma diagnosed in the VA each year—and is likely an underestimate, DuMontier explained.
A study he led examined national VA data that identified all veterans newly diagnosed with multiple myeloma who initiated treatment in VAMCs with either the triplet bortezomib-lenalidomide-dexamethasone (VRd) or the doublet lenalidomide-dexamethasone (Rd) from the years 2004 to 2020. Veterans who received transplants within the initial months of treatment were excluded.
“Our study found that the more intensive triplet bortezomib-lenalidomide-dexamethasone was associated with a greater benefit in veterans compared to the less intensive doublet lenalidomide-dexamethasone—confirming clinical trial evidence,” DuMontier said. “This benefit was even more pronounced in veterans with the highest levels of frailty, challenging the historical expert opinion-based recommendation to consider the doublet over the triplet in patients who are frail.”
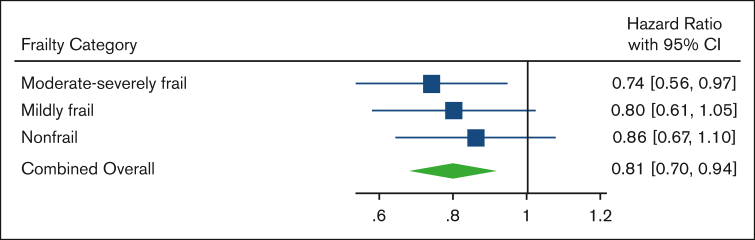
Click to Enlarge: Mortality of VRd vs. Rd within each frailty category and in combined overall population. Forest plot of HRs and 95% CIs from Cox proportional hazards models evaluating association of VRd vs Rd with mortality, based on frailty severity and in the combined overall population after matching or stage and PS within frailty categories. Source: Blood Advances
“In general, frailty is viewed as a measure of treatment tolerability, whereby the frailer a patient is, the higher the risk of toxicity from treatment. The historical concern in frail patients is that the risk of toxicity associated with a more-intensive triplet regimen vs. a less intensive doublet regimen would outweigh the benefit of better myeloma control,” he pointed out.
The study found, however, that “frail veterans had better survival when treated with the triplet therapy compared to the doublet therapy, contrary to the historical recommendation to consider the doublet over the triplet in this population,” DuMontier suggested.
When looking at the health deficits contributing to frailty in this veteran population, myeloma-related complications (low blood counts, bone disease, kidney disease) and aggressive (stage III) myeloma were more prevalent in patients who were moderate-severely frail than in those who were nonfrail, he added, explaining, “Moreover, these myeloma-related deficits were more prevalent in patients who were frail in the current study than in those in the more general veteran population. Multiple myeloma and its complications likely drive this higher prevalence of frailty, and as frailty increases, myeloma and its complications contribute disproportionately more to frailty than other, nononcologic frailty deficits. Therefore, more intensive (e.g., borteomib-lenalidomide-dexamethasone) vs. less intensive (e.g., lenalidomide-dexamethasone) treatment for a veteran who is frail with multiple myeloma may actually deliver more effective treatment of frailty itself.”
The authors sought to explore this topic because, “the optimal intensity of treatment in adults who are frail with multiple myeloma is often uncertain, given the higher risk of harm in patients who are frail and treated with standard, intensive regimens,” DuMontier said.
“Randomized controlled trials directly or indirectly exclude patients who are frail, limiting the generalizability of results to a large portion of patients treated in practice,” he advised. “Veterans are even more underrepresented in clinical trials than the general population. We designed this study to test the assumption that the benefit of the triplet lenalidomide-bortezomib-dexamethasone diminished in frail patients. Studies that can observe ‘real-world’ outcomes among different treatment regimens can fill the gap in evidence left by clinical trials in nonrepresentative populations.”
The authors recommended that “all veterans with multiple myeloma receive a frailty assessment at diagnosis.” In addition, they recommend that “frailty not merely be viewed as a measure of treatment tolerability but more broadly as a summary measure of a patient’s health status that reflects both cancer and noncancer contributors,” according to the authors.
“Distinguishing myeloma-related versus nononcologic, aging-related contributors to frailty can help determine whether patients derive a net benefit or net harm on more intensive novel regimens when there is evidence lacking from clinical trial populations regarding the safety and effectiveness of these regimens in frail patients treated in practice,” DuMontier said. “In this way, frailty does not imply that less intensive regimens should be used, but rather that treatment of multiple myeloma as a contributor of frailty may be treatment of frailty itself. Reevaluating frailty in follow-up alongside reevaluating biochemical markers of myeloma can help determine whether a patient is improving in their health status, thus testing the oncologist’s initial ‘hypothesis’ about what was driving the patient’s frailty.”
Thanks to innovation in treatment, patients newly diagnosed with multiple myeloma can live an average of 10 years or longer. Besides Rd and VRd, newer, better-tolerated triplet regimens, such as daratumumab-lenalidomide-dexamethasone, are other options that are now more commonly prescribed in veterans, DuMontier said.
“We are even beginning to see the use of quadruplet (four-drug) regimens, and novel treatments such as bispecific T-cell engager (BiTE) therapies for veterans who have relapsed on prior therapies and until recently had little other options,” he added. “As with our current study of bortezomib-lenalidomide-dexamethasone, the safety and effectiveness of these therapies should be confirmed as they are more widely used in the veteran population. Just because we found that a triplet regimen over a doublet regimen carries a net benefit in frail veterans, does not mean that we will find the same net benefit in frail patients treated with a quadruplet regimen over a triplet regimen.”
- DuMontier C, La J, Bihn J, Corrigan J, et. Al. More intensive therapy as more effective treatment for frail patients with multiple myeloma [corrected]. Blood Adv. 2023 Oct 24;7(20):6275-6284. doi: 10.1182/bloodadvances.2023011019. Erratum in: Blood Adv. 2023 Nov 28;7(22):7100. PMID: 37582048; PMCID: PMC10589796.
