Once called the “disease of kings,” gout no longer has an association with wealth and indulgence. In reality, its prevalence is higher in men and older patients, and it affects military veterans treated at the VA more than patients in the community. It also is on the rise, something that especially concerns researchers.
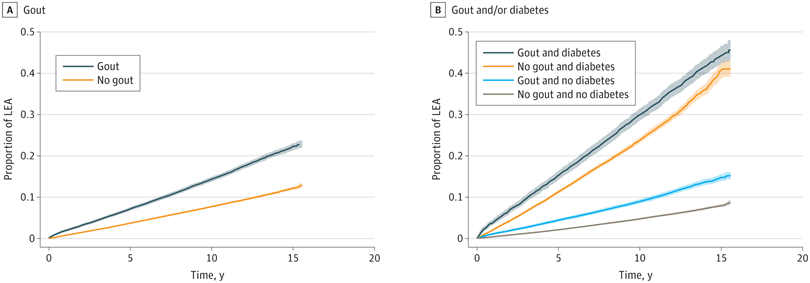
Click to Enlarge: Cumulative incidence estimates using Cox proportional hazards regression models and based on the presence of gout and the dual presence of gout and/or diabetes. The overall Cox proportional hazards regression model was adjusted for age, sex, race and ethnicity, body mass index, smoking history, and comorbidities (hypertension, cardiovascular disease, peripheral artery disease, cancer, cerebrovascular disease, chronic lung disease, dementia, diabetes, and kidney disease). The model of dual associations of gout and/or diabetes was adjusted for the same covariates, with the exception of diabetes. Shaded areas indicate 95% CIs. Source: JAMA Network Open
OMAHA, NE — One of the earliest recorded and most intensely painful diseases, gout was historically called the “disease of kings.” For centuries, it was thought to affect only the wealthy and aristocratic.
Although gout’s painful reputation (some say merely the pressure of a bedsheet or a breeze on an inflamed joint can be excruciating) has persisted, its association with wealth and indulgence has been challenged and refuted.
Clinical experience and research, including studies in veterans, have painted a different picture—one that affects all socioeconomic classes, with certain groups being more vulnerable to uncontrolled gout and its serious complications.
Concerning Findings in Veterans
Concerningly, the prevalence of gout has risen in recent years, and it appears to affect veterans disproportionately.
In a 2020 study examining the prevalence and burden of gout in the veteran population, researchers led by rheumatologist Lindsay N. Helget, MD, of the Omaha, NE, VA Medical Center found that, in 2014, the prevalence of gout in the VHA was 5.8% compared to 4.2% in 2005. Gout prevalence was highest among men, older patients and non-Hispanic black patients. During 2014, 4.0% of all inpatient or outpatient encounters and 1.3% of hospitalizations were gout-related.1
“Gout is a problem everywhere, not just for the veteran population,” Helget told the Compendium of Federal Medicine. “However, when comparing the findings of our paper to the findings in other studies, there does appear to be a substantially higher prevalence—5.8% in the VA compared to almost 4% in another national U.S. study—suggesting that, by crude numbers alone, gout is an even bigger problem in our veterans than the general population.”
Although Helget said she and her colleagues have no updated figures from the original study, based on other estimates in the United States and other parts of the world, she thinks “it’s very likely that this prevalence has continued to increase over time.”
A ‘Curable’ Disease That Goes Uncured
Gout occurs when excess uric acid deposits as needle-sharp crystals in the joints. Uncontrolled, gout can become chronic, punctuated by periodic attacks on joints.
In theory, gout can be cured when treatment with appropriate urate-lowering therapies (allopurinol and febuxostat) achieves a goal uric acid of 6mg/dL or lower.
Other treatment options include probenecid, which increases the renal excretion of uric acid, and for treatment-resistant gout, IV pegloticase, which rapidly breaks down uric acid into more soluble compounds that the body can more easily eliminate, Helget said.
But, due to underutilization of appropriate treatment and other factors, many people never achieve that goal.
While uncontrolled gout is an issue across all patient populations, researchers have found that “attaining treatment goals with serum urate is more challenging in non-white populations—for yet unknown reasons—suggesting we need to pay specific attention to this population when treating gout,” said Helget. “These populations include Black/African Americans, Asian, Native Hawaiian/Pacific Islander and American Indians.”
A study presented at the American College of Rheumatology’s annual scientific meeting by researchers at the VA Portland, OR, Healthcare System found that gout also tended to be poorly controlled in patients living in rural areas. In the study of 2,421 veterans who were identified as having gout and received care at VA in 2019 with VA Northwest Network (VISN 20), only one-third of those identified as living in rural areas had controlled gout using serum urate levels. The authors stated that “interventions that share rheumatology best practices and expertise for managing gout with VA primary care teams, such as the VA Rheumatology Extension for Community Healthcare Outcomes ECHO program and expansion of telehealth within VA rheumatology, should be developed and tested to enhance quality of care for rural veterans.”2
More Than Painful Joints
Painful gout attacks are often treated with opioids, Helget’s prevalence study showed. In 2014, 16.4% of prevalent gout patients were receiving a weak opioid, nearly doubling the prescription rate of weak opioids in 2005, a finding Helget found particularly surprising—and concerning.1
Although her group have not examined figures beyond 2014, she said, “we have done additional analyses of this data within the same time frame which showed that nearly 60% of gout patients receive an opioid at some point in their disease course and that gout patients were 36% more likely than those without gout to receive opioids leading to chronic opioid use.”3
Frequent gout attacks that occur when serum uric acid levels are not controlled can cause irreparable damage to the joints. Other complications include tophi, accumulations of monosodium urate in the soft tissues, synovial tissues or bones near the joints; kidney stones; kidney disease and even kidney failure. One study in veterans found suboptimal serum urate control was also associated with a higher rate of lower extremity amputations in patients with gout.4
Even more concerning is that uncontrolled gout is associated with increased mortality. “We do not specifically have those numbers, but we have found that gout patients in the VA whose gout is ‘suboptimally’ treated, meaning they did not recurrently fill their gout treatment medications or reach control of their serum urate, had a 22% increased risk of mortality compared to VA patients with gout who were considered to be well controlled—[meaning they] refilled their gout medications and met their uric acid goals,” she said.5
Appropriate Management is Crucial
“The overall take home message of our findings is that gout afflicts a large number of patients in the Veteran’s Health Administration, and therefore we need to be taking steps to ensure these patients are identified and treated appropriately,” Helget said. “Gout is a chronic condition requiring chronic management. Ideally, to ensure its optimal long-term management, gout should be viewed no differently than any other chronic conditions for which you have regular follow-up appointments for management.”
“We have incredibly effective treatments, which can help the vast majority of patients manage their gout. A long-term approach needs to be the standard of care in gout management to ensure that medications are working, dosing is appropriate, and patients are compliant with prescribed therapies,” she said.
- Helget, L. N., England, B. R., Roul, P., Sayles, H., Petro, A. D., Michaud, K., & Mikuls, T. R. (2021). Incidence, Prevalence, and Burden of Gout in the Veterans Health Administration. Arthritis care & research, 73(9), 1363–1371. https://doi.org/10.1002/acr.24339
- Barton, J., Larsen, C., Matsumoto, R., & O’Neill, A. (2021). Rural veterans with gout – “Rheum” for improvement. ACR Meeting Abstracts. https://acrabstracts.org/abstract/rural-veterans-with-gout-rheum-for-improvement/
- Barton, J., Larsen, C., Matsumoto, R., & O’Neill, A. (2021). Rural veterans with gout – “Rheum” for improvement. ACR Meeting Abstracts. https://acrabstracts.org/abstract/rural-veterans-with-gout-rheum-for-improvement/
- Mikuls, T. R., Soto, Q., Petro, A., Helget, L., Roul, P., Sayles, H., Cope, B., Neogi, T., LaMoreaux, B., O’Dell, J. R., & England, B. R. (2022). Comparison of Rates of Lower Extremity Amputation in Patients With and Without Gout in the US Department of Veterans Affairs Health System. JAMA network open, 5(1), e2142347. https://doi.org/10.1001/jamanetworkopen.2021.42347
- Arthritis & Rheumatism. (2021b). Mortality in patients with sub-optimally treated gout in the Veteran’s Health Administration: A national retrospective cohort study. ACR Meeting Abstracts. https://acrabstracts.org/abstract/mortality-in-patients-with-sub-optimally-treated-gout-in-the-veterans-health-administration-a-national-retrospective-cohort-study/
