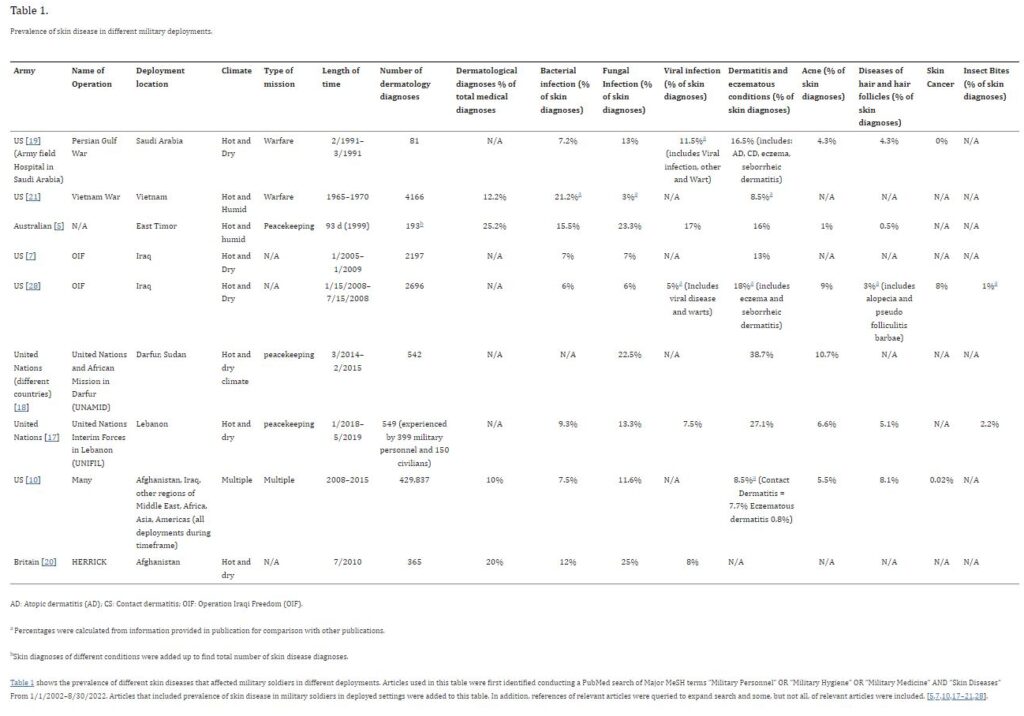
Click to Enlarge: AD: Atopic dermatitis (AD); CS: Contact dermatitis; OIF: Operation Iraqi Freedom (OIF).
a. Percentages were calculated from information provided in publication for comparison with other publications.
b. Skin diagnoses of different conditions were added up to find total number of skin disease diagnoses.
Table 1 shows the prevalence of different skin diseases that affected military soldiers in different deployments. Articles used in this table were first identified conducting a PubMed search of Major MeSH terms “Military Personnel” OR “Military Hygiene” OR “Military Medicine” AND “Skin Diseases” From 1/1/2002–8/30/2022. Articles that included prevalence of skin disease in military soldiers in deployed settings were added to this table. In addition, references of relevant articles were queried to expand search and some, but not all, of relevant articles were included. Source: Taylor & Francis – Annals of Medicine
Military servicemembers are often exposed to drastic climates, environments, and living conditions which may make them more susceptible to cutaneous diseases, according to a new study.
Researchers from Rutgers, New Jersey Medical School and Weill Cornell Medicine in New York said that is a serious concern for the about 1.2 million active-duty members and 780,000 reservists in the U.S. forces.
The study team conducted a PubMed search of studies published between Jan. 1, 2002, and Aug. 30, 2022, using MeSH terms: “Military Personnel” [Majr] OR “Military Hygiene” [Majr] OR “Military Medicine” [Majr] AND “Skin Diseases” [Majr] and also reviewed the reference lists of select articles, and other applicable sources to identify articles on skin conditions affecting military soldiers and treatment options.
In an article in Annals of Medicine, the authors reviewed skin conditions that affect military soldiers in both the deployed and non-deployed settings. Those included infectious diseases, arthropod-associated diseases, sexually transmitted infections, ultraviolet radiation related skin disease, acne, diseases of hair and hair follicles, dermatitis, onychocryptosis, and conditions caused by extreme weather conditions and occupational exposures. Treatment options and prevention methods are also discussed in terms of military settings.1
“Dermatological conditions can considerably impact soldiers’ wellbeing and military performance, often lead to evacuation of military personnel, and are associated with high financial costs,” the study noted. “Cutaneous disease is one of the most common reasons for soldiers to seek medical care and may cause significant morbidity. Serving in the military often impacts and limits treatment options.”
The researchers provided two key pieces of advice for healthcare providers:
- Military soldiers are a unique population exposed to crowded living conditions, reduced opportunity for personal hygiene, environmental contamination, strict grooming practices, and skin injury which may contribute to infectious and arthropod-associated skin, hair, and nail diseases in soldiers.
- Treatment options for skin diseases that are commonly used in the general population may have implications for military duties that should be considered before treatment initiation in soldiers.
“Skin diseases often lead to evacuation of military personnel from combat theater and affect soldier training and morale,” the researchers explained. “Cutaneous disease related disruptions in the military not only hinder military operations but are also associated with high financial costs. In a study on teledermatology consults of deployed U.S. soldiers in Iraq 1/2005–1/2009, the cost of evacuating soldiers back to the US was estimated at $562,380 and the cost of in-person dermatology evaluations in Iraq was $416,000.”
Among the challenges of treating skin conditions in deployed soldiers include slow turnaround time for pathology specimens, lack of access to dermatological care, and arranging follow up care, they added.
The report specifically addressed atopic dermatitis, noting “Diagnosis of atopic dermatitis (AD) after the 12th birthday is a disqualifying medical criterion for enlistment in the US military, though mild and well controlled cases often receive a waiver. AD often flares in soldiers [6], and correlates with stress levels experienced in the military.”
The authors cited a Korean study that found that stress levels (measured with a 14-part questionnaire) were associated with both AD and seborrheic dermatitis (SD). “Furthermore, environmental factors and lack of access to certain care measures, such as regular baths and moisturizers, can exacerbate AD in soldiers,” they wrote. “AD can cause ocular complications and poses a risk for secondary infections, which can be especially problematic in military settings.”
The study advised that treatment options of AD in soldiers “include emollients, cleansers, and topical steroids and immunomodulators, and biologics. UV therapy can be used in non-deployed settings. Immunosuppressant use in soldiers is limited to short-term treatment due to their side effect profiles, need for laboratory monitoring, and immunosuppression.”
The authors pointed out that that mortality from skin disease in military personnel is low, but dermatologic conditions in the military setting make up a proportion of servicemember morbidity. “In a review of skin conditions in military peacekeeping operations, military physician visits for skin conditions ranged from 9.3% (during the Gulf war) to 25.2% (in an East Timor deployment),” they wrote. “In US soldiers specifically, 10% (429,837 cases) of deployed setting medical diagnoses 2008–2015, were dermatological.”
- Singal A, Lipner SR. A review of skin disease in military soldiers: challenges and potential solutions. Ann Med. 2023;55(2):2267425. doi: 10.1080/07853890.2023.2267425. Epub 2023 Oct 16. PMID: 37844200; PMCID: PMC10580865.

